url?sa=t&source=web&cd=2&ved=0CC0QFjAB&url=http://filletofish.net/usc/Pocket_Medicine_4th_Edition
url?sa=t&source=web&cd=2&ved=0CC0QFjAB&url=http://filletofish.net/usc/Pocket_Medicine_4th_Edition
url?sa=t&source=web&cd=2&ved=0CC0QFjAB&url=http://filletofish.net/usc/Pocket_Medicine_4th_Edition
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
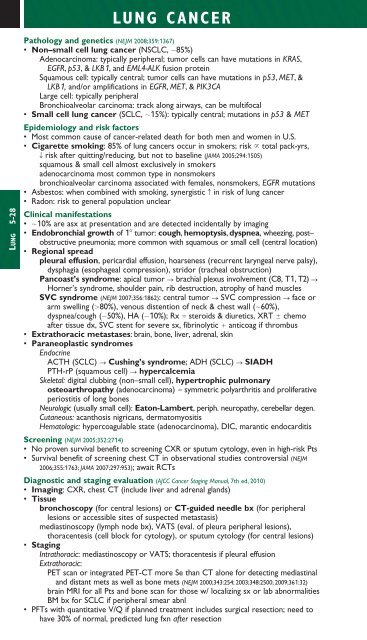
LUNG CANCERLUNG 5-28Pathology and ge<strong>net</strong>ics (NEJM 2008;359:1367)• Non–small cell lung cancer (NSCLC, 85%)Adenocarcinoma: typically peripheral; tumor cells can have mutations in KRAS,EGFR, p53, & LKB1, and EML4-ALK fusion proteinSquamous cell: typically central; tumor cells can have mutations in p53, MET, &LKB1, and/or amplifications in EGFR, MET, & PIK3CALarge cell: typically peripheralBronchioalveolar carcinoma: track along airways, can be multifocal• Small cell lung cancer (SCLC, 15%): typically central; mutations in p53 & METEpidemiology and risk factors• Most common cause of cancer-related death for both men and women in U.S.• Cigarette smoking: 85% of lung cancers occur in smokers; risk total pack-yrs,T risk after quitting/reducing, but not to baseline (JAMA 2005;294:1505)squamous & small cell almost exclusively in smokersadenocarcinoma most common type in nonsmokersbronchioalveolar carcinoma associated with females, nonsmokers, EGFR mutations• Asbestos: when combined with smoking, synergistic c in risk of lung cancer• Radon: risk to general population unclearClinical manifestations• 10% are asx at presentation and are detected incidentally by imaging• Endobronchial growth of 1 tumor: cough, hemoptysis, dyspnea, wheezing, post–obstructive pneumonia; more common with squamous or small cell (central location)• Regional spreadpleural effusion, pericardial effusion, hoarseness (recurrent laryngeal nerve palsy),dysphagia (esophageal compression), stridor (tracheal obstruction)Pancoast’s syndrome: apical tumor S brachial plexus involvement (C8, T1, T2) SHorner’s syndrome, shoulder pain, rib destruction, atrophy of hand m<strong>usc</strong>lesSVC syndrome (NEJM 2007;356:1862): central tumor S SVC compression S face orarm swelling (80%), venous distention of neck & chest wall (60%),dyspnea/cough (50%), HA (10%); Rx steroids & diuretics, XRT chemoafter tissue dx, SVC stent for severe sx, fibrinolytic anticoag if thrombus• Extrathoracic metastases: brain, bone, liver, adrenal, skin• Paraneoplastic syndromesEndocrineACTH (SCLC) S Cushing’s syndrome; ADH (SCLC) S SIADHPTH-rP (squamous cell) S hypercalcemiaSkeletal: digital clubbing (non–small cell), hypertrophic pulmonaryosteoarthropathy (adenocarcinoma) symmetric polyarthritis and proliferativeperiostitis of long bonesNeurologic (usually small cell): Eaton-Lambert, periph. neuropathy, cerebellar degen.Cutaneous: acanthosis nigricans, dermatomyositisHematologic: hypercoagulable state (adenocarcinoma), DIC, marantic endocarditisScreening (NEJM 2005;352:2714)• No proven survival benefit to screening CXR or sputum cytology, even in high-risk Pts• Survival benefit of screening chest CT in observational studies controversial (NEJM2006;355:1763; JAMA 2007;297:953); await RCTsDiagnostic and staging evaluation (AJCC Cancer Staging Manual, 7th ed, 2010)• Imaging: CXR, chest CT (include liver and adrenal glands)• Tissuebronchoscopy (for central lesions) or CT-guided needle bx (for peripherallesions or accessible sites of suspected metastasis)mediastinoscopy (lymph node bx), VATS (eval. of pleura peripheral lesions),thoracentesis (cell block for cytology), or sputum cytology (for central lesions)• StagingIntrathoracic: mediastinoscopy or VATS; thoracentesis if pleural effusionExtrathoracic:PET scan or integrated PET-CT more Se than CT alone for detecting mediastinaland distant mets as well as bone mets (NEJM 2000;343:254; 2003;348:2500; 2009;361:32)brain MRI for all Pts and bone scan for those w/ localizing sx or lab abnormalitiesBM bx for SCLC if peripheral smear abnl• PFTs with quantitative V/Q if planned treatment includes surgical resection; need tohave 30% of normal, predicted lung fxn after resection