MECH VENT 2-20Step 3: Set or ✓ Remaining VariablesF iO 2 Fraction of inspired air that is oxygenPositive Positive pressure applied during exhalation via resistor in exhalation portend- Benefits: prevents alveoli collapse, T intrapulmonary shunt, c O 2expiratory Cardiac effects: T preload by c intrathoracic pressure STvenous return;pressureT afterload by T cardiac transmural pressure; may c or T CO and may c or(PEEP)T oxygen delivery based on the aboveAuto-PEEP or intrinsic PEEP: inadequate exhalation time S lungsunable to completely empty before the next breath (ie,“breathstacking”); if flow at end-expiration, there must be pressure auto-PEEPWill T preload and may T CO, especially if hypovolemicWill c work of breathing as must be overcome by Pt to trigger breaths;can prevent Pt from successfully triggering ventilatorCan be detected if end-expiratory flow Z 0 before next breathCan measure by occluding expiratory port of vent at end-expirationCan T by: c exp time, T RR, T V T, Rx bronchospasm and secretionsInspiratory Normally I:E ratio is 1:2; however, can alter I time (and consequentlytimeflow rate, see later); use in pressure-control modeInspiratory c flow rate STI time ScE time S ∴ may improve ventilation in obstructiveflow rates disease, but may affect resp rate and bronchodilation/constrictionPeak Dynamic measurement during inspiration; set in pressure-targeted modeinspiratory Determined by airway resistance and lung/chest wall compliancepressure c PIP w/o c P plat Scairway resist (eg, bronchospasm, plugging)(PIP)T PIP STairway resistance or air leak in the systemPlateau Static measurement at the end of inspiration when there is no flowpressure Determined by resp system compliance (resist. not a factor since ∅ flow)(P plat) c P plat STlung or chest wall compliance (eg, PTX, pulmonary edema,pneumonia, atelectasis), c PEEP, or auto-PEEPP plat 30 cm H 2O T barotrauma (T V T, T PEEP or c compl [eg, by diuresis])Initial SettingsMode Tidal volume Respiratory rate F iO 2 PEEPAssist control 4–8 * mL/kg 12–14 1.0 (ie, 100%) ? 5 cm H 2Ovolume-targeted IBW breaths/min* Goal for ARDS; ventilation at VT 8 mL/kg may be injurious in other types of ventilated Pts as well.Noninvasive VentilationConditionsCardiogenic pulmonary edema: may T intub. & mortality (JAMA2005;294:3124; Lancet 2006;367:1155) although recent trial (w/ highcrossover) did not show any benefit (NEJM 2008;359:142)COPD exacerbation w/ hypercapnia: T intub. & mortality (Lancet2000;355:1931), but if pH 7.3 S intubateHigh-risk extubation (age 65, CHF,APACHE II 12): NIV 24 hdirectly after extubation STreintub and, if P aCO 2 45 duringSBT, T mortality (AJRCCM 2006;173:164). However, if used asrescue after failed extubation Scmortality (NEJM 2004;350:2452).End-of-life care (Resp Care 2009;54:223)Immunosupp. w/ infiltrates: T complic & mort (NEJM 2001;344:481)IndicationsClinical: mod-severe dyspnea, RR 24–30, signs of c work of(Lancet 2009;374:250) breathing, accessory m<strong>usc</strong>le use, abd paradoxGas exchange:P aCO 2 45 (& significantly worse than baseline),hypoxemia, P aO 2/F iO 2 200Contraindications Claustrophobia, inability to fit mask, MS, vomiting, unable to(JAMA 2002;288:932) protect airway, extrapulm organ failure, hemodyn instab, sev UGIBContinuous positive PEEPairway pressure No limit on O 2 delivered (ie, can give hi-flow S F iO 2 1.0)(CPAP)Used if primary problem hypoxemia (eg, CHF)NPPV/bilevel PSV PEEP.Able to set both inspiratory (usually 8–10 cm H 2O)positive airway and expiratory pressures (usually 5 cm H 2O).pressure (BiPAP) Used if primary problem hypoventilation;F iO 2 delivery limitedMask ventilation Tight-fitting mask connecting patient to a standard ventilatorCan receive PS 20–30 cm H 2O, PEEP 10 cm H 2O, F iO 2 1.0Used for short-term support (24 h) for a reversible process
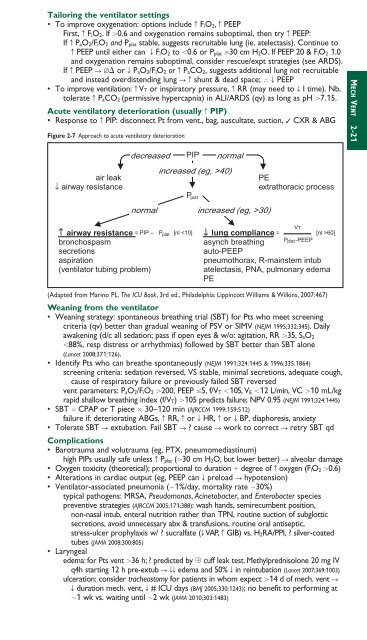
Tailoring the ventilator settings• To improve oxygenation: options include c F iO 2, c PEEPFirst, c F iO 2. If 0.6 and oxygenation remains suboptimal, then try c PEEP:If c P aO 2/F iO 2 and P plat stable, suggests recruitable lung (ie, atelectasis). Continue toc PEEP until either can T F iO 2 to 0.6 or P plat 30 cm H 2O. If PEEP 20 & F iO 2 1.0and oxygenation remains suboptimal, consider rescue/expt strategies (see ARDS).If c PEEP S ∅ or T P aO 2/F iO 2 or c P aCO 2, suggests additional lung not recruitableand instead overdistending lung Scshunt & dead space; ∴ T PEEP• To improve ventilation: c V T or inspiratory pressure, c RR (may need to T I time). Nb,tolerate c P aCO 2 (permissive hypercapnia) in ALI/ARDS (qv) as long as pH 7.15.Acute ventilatory deterioration (usually c PIP)• Response to c PIP: disconnect Pt from vent., bag, a<strong>usc</strong>ultate, suction, ✓ CXR & ABGFigure 2-7 Approach to acute ventilatory deteriorationair leak↓ airway resistancedecreasedPIPincreased (eg, >40)Pnormalnormal increased (eg, >30)PEextrathoracic processMECH VENT 2-21↑ airway resistance = PIP – P [nl 60]asynch breathingauto-PEEPP -PEEPpneumothorax, R-mainstem intubatelectasis, PNA, pulmonary edemaPEVT(Adapted from Marino PL. The ICU Book, 3rd ed., Philadelphia: Lippincott Williams & Wilkins, 2007:467)Weaning from the ventilator• Weaning strategy: spontaneous breathing trial (SBT) for Pts who meet screeningcriteria (qv) better than gradual weaning of PSV or SIMV (NEJM 1995;332:345). Dailyawakening (d/c all sedation; pass if open eyes & w/o: agitation, RR 35, S aO 288%, resp distress or arrhythmias) followed by SBT better than SBT alone(Lancet 2008;371:126).• Identify Pts who can breathe spontaneously (NEJM 1991;324:1445 & 1996;335:1864)screening criteria: sedation reversed, VS stable, minimal secretions, adequate cough,cause of respiratory failure or previously failed SBT reversedvent parameters: P aO 2/F iO 2 200, PEEP 5, f/V T 105, V E 12 L/min, VC 10 mL/kgrapid shallow breathing index (f/V T) 105 predicts failure; NPV 0.95 (NEJM 1991;324:1445)• SBT CPAP or T piece 30–120 min (AJRCCM 1999;159:512)failure if: deteriorating ABGs, c RR, c or T HR, c or T BP, diaphoresis, anxiety• Tolerate SBT S extubation. Fail SBT S ? cause S work to correct S retry SBT qdComplications• Barotrauma and volutrauma (eg, PTX, pneumomediastinum)high PIPs usually safe unless c P plat (30 cm H 2O, but lower better) S alveolar damage• Oxygen toxicity (theoretical); proportional to duration degree of c oxygen (F iO 2 0.6)• Alterations in cardiac output (eg, PEEP can T preload S hypotension)• Ventilator-associated pneumonia (1%/day, mortality rate 30%)typical pathogens: MRSA, Pseudomonas, Aci<strong>net</strong>obacter, and Enterobacter speciespreventive strategies (AJRCCM 2005;171:388): wash hands, semirecumbent position,non-nasal intub, enteral nutrition rather than TPN, routine suction of subglotticsecretions, avoid unnecessary abx & transfusions, routine oral antiseptic,stress-ulcer prophylaxis w/ ? sucralfate (T VAP, c GIB) vs. H 2RA/PPI, ? silver-coatedtubes (JAMA 2008;300:805)• Laryngealedema: for Pts vent 36 h; ? predicted by cuff leak test. Methylprednisolone 20 mg IVq4h starting 12 h pre-extub STTedema and 50% T in reintubation (Lancet 2007;369:1003)ulceration: consider tracheostomy for patients in whom expect 14 d of mech. vent ST duration mech. vent, T # ICU days (BMJ 2005;330:1243); no benefit to performing at1 wk vs. waiting until 2 wk (JAMA 2010;303:1483)
- Page 3 and 4:
POCKETNOTEBOOKPocketMEDICINEFourth
- Page 5 and 6:
Contributing AuthorsForewordPreface
- Page 7 and 8:
HIV/AIDS 6-17Tick-Borne Diseases 6-
- Page 9 and 10:
Rajat Gupta, MDInternal Medicine Re
- Page 11 and 12:
FOREWORDTo the 1st EditionIt is wit
- Page 13 and 14:
ELECTROCARDIOGRAPHYApproach (a syst
- Page 15 and 16:
CHEST PAINDisorderUnstableanginaMIP
- Page 17 and 18:
CORONARY ANGIOGRAPHY AND REVASCULAR
- Page 19 and 20:
Likelihood of ACSFeature High Inter
- Page 21 and 22:
STEMIReperfusion• Immediate reper
- Page 23 and 24: • VT/VF: lido or amio 6-24 h, th
- Page 25 and 26: PA Catheter WaveformsLocation RA RV
- Page 27 and 28: Evaluation of the causes of heart f
- Page 29 and 30: CARDIOMYOPATHIESDiseases with mecha
- Page 31 and 32: RESTRICTIVE CARDIOMYOPATHY (RCMP)De
- Page 33 and 34: AORTIC INSUFFICIENCY (AI)Etiology (
- Page 35 and 36: Clinical manifestations (Lancet 200
- Page 37 and 38: PERICARDIAL DISEASEGENERAL PRINCIPL
- Page 39 and 40: CONSTRICTIVE PERICARDITISEtiology
- Page 41 and 42: • Pharmacologic options (if HTN o
- Page 43 and 44: ACUTE AORTIC SYNDROMESDefinitions (
- Page 45 and 46: OnsetRateRhythmP wavemorphologyResp
- Page 47 and 48: ATRIAL FIBRILLATIONClassification (
- Page 49 and 50: SYNCOPEDefinition• Symptom of sud
- Page 51 and 52: INTRACARDIAC DEVICESPacemaker CodeA
- Page 53 and 54: Pre-operative testing and therapy
- Page 55 and 56: DYSPNEAPathophysiologyEtiologiesAir
- Page 57 and 58: Other• Behavior modification: ide
- Page 59 and 60: CHRONIC OBSTRUCTIVE PULMONARY DISEA
- Page 61 and 62: HEMOPTYSISDefinition and pathophysi
- Page 63 and 64: INTERSTITIAL LUNG DISEASEWORKUP OF
- Page 65 and 66: PLEURAL EFFUSIONPathophysiology•
- Page 67 and 68: VENOUS THROMBOEMBOLISM (VTE)Definit
- Page 69 and 70: Risk stratification for Pts with PE
- Page 71 and 72: • SupportiveOxygen: maintain S aO
- Page 73: MECHANICAL VENTILATIONIndications
- Page 77 and 78: SEPSISDefinitionsSystemic2 or more
- Page 79 and 80: ESOPHAGEAL AND GASTRIC DISORDERSDYS
- Page 81 and 82: GASTROINTESTINAL BLEEDINGDefinition
- Page 83 and 84: DIARRHEA, CONSTIPATION, AND ILEUSAC
- Page 85 and 86: Dx: IgA antitissue transglutaminase
- Page 87 and 88: DIVERTICULAR DISEASEDIVERTICULOSISD
- Page 89 and 90: MANAGEMENT (Lancet 2007;369:1641 &
- Page 91 and 92: PANCREATITISPathogenesis• Acinar
- Page 93 and 94: ABNORMAL LIVER TESTSTests of hepato
- Page 95 and 96: HEPATITISVIRALHepatitis A (ssRNA; a
- Page 97 and 98: AUTOIMMUNE HEPATITIS (AIH)Classific
- Page 99 and 100: CIRRHOSISDefinition (Lancet 2008;37
- Page 101 and 102: PrognosisModified Child-Turcotte-Pu
- Page 103 and 104: HEPATIC VASCULAR DISEASEPortal vein
- Page 105 and 106: BILIARY TRACT DISEASECHOLELITHIASIS
- Page 107 and 108: ACID-BASE DISTURBANCESGENERALDefini
- Page 109 and 110: Workup for AG metabolic acidosis•
- Page 111 and 112: Etiologies of Metabolic AlkalosisSa
- Page 113 and 114: Hypovolemic hypotonic hyponatremia
- Page 115 and 116: POLYURIADefinition and pathophysiol
- Page 117 and 118: Treatment• If true potassium defi
- Page 119 and 120: Treatment• Treat underlying disor
- Page 121 and 122: DIALYSISGeneral• Substitutes for
- Page 123 and 124: Treatment• ANCA or anti-GBM: ste
- Page 125 and 126:
HEMATURIAEtiologies of HematuriaExt
- Page 127 and 128:
ANEMIAT in RBC mass: Hct 41% or Hb
- Page 129 and 130:
MACROCYTIC ANEMIASincludes megalobl
- Page 131 and 132:
• Infection: splenic infarction S
- Page 133 and 134:
PLATELET DISORDERSTHROMBOCYTOPENIA
- Page 135 and 136:
• Treatment of type II (NEJM 2006
- Page 137 and 138:
HYPERCOAGULABLE STATESSuspect in Pt
- Page 139 and 140:
TRANSFUSION THERAPYPacked red blood
- Page 141 and 142:
MYELOPROLIFERATIVE NEOPLASMS (MPN)G
- Page 143 and 144:
LEUKEMIAACUTE LEUKEMIADefinition•
- Page 145 and 146:
Prognosis• CR achieved in 80% of
- Page 147 and 148:
LYMPHOMADefinition• Malignant dis
- Page 149 and 150:
Consider CNS prophylaxis w/ intrath
- Page 151 and 152:
Treatment (NEJM 2004;351:1860; Lanc
- Page 153 and 154:
• Sinusoidal obstruction syndrome
- Page 155 and 156:
TNM Staging System for NSCLCN stage
- Page 157 and 158:
Simplified Staging System for Breas
- Page 159 and 160:
COLORECTAL CANCER (CRC)Epidemiology
- Page 161 and 162:
PANCREATIC TUMORSPathology and gene
- Page 163 and 164:
• Prostate, breast, and lung canc
- Page 165 and 166:
PNEUMONIAMicrobiology of PneumoniaC
- Page 167 and 168:
FUNGAL INFECTIONSCandida species•
- Page 169 and 170:
URINARY TRACT INFECTIONS (UTI)Defin
- Page 171 and 172:
Diagnostic studies• Superficial s
- Page 173 and 174:
INFECTIONS OF THE NERVOUS SYSTEMACU
- Page 175 and 176:
VIRAL ENCEPHALITISDefinition• Vir
- Page 177 and 178:
Diagnostic studies• Blood culture
- Page 179 and 180:
TUBERCULOSISEpidemiology• U.S.: 1
- Page 181 and 182:
HIV/AIDSDefinition• AIDS: HIV CD
- Page 183 and 184:
Cutaneous• Seborrheic dermatitis;
- Page 185 and 186:
TICK-BORNE DISEASESDistinguishing F
- Page 187 and 188:
FEVER OF UNKNOWN ORIGIN (FUO)Defini
- Page 189 and 190:
PITUITARY DISORDERSHYPOPITUITARY SY
- Page 191 and 192:
THYROID DISORDERSDiagnostic Studies
- Page 193 and 194:
Clinical manifestations of hyperthy
- Page 195 and 196:
ADRENAL DISORDERSCushing’s Syndro
- Page 197 and 198:
Treatment• Adenoma or carcinoma S
- Page 199 and 200:
CALCIUM DISORDERSLaboratory Finding
- Page 201 and 202:
DIABETES MELLITUSDefinition (Diabet
- Page 203 and 204:
Typical DKA “Flow sheet” SetupV
- Page 205 and 206:
ARTHRITIS—OVERVIEWApproach to pat
- Page 207 and 208:
RHEUMATOID ARTHRITIS (RA)Definition
- Page 209 and 210:
CRYSTAL DEPOSITION ARTHRITIDESGOUTD
- Page 211 and 212:
SERONEGATIVE SPONDYLOARTHRITISGENER
- Page 213 and 214:
INFECTIOUS ARTHRITIS & BURSITISDIAG
- Page 215 and 216:
CONNECTIVE TISSUE DISEASES% Autoant
- Page 217 and 218:
Clinical manifestations• Muscle w
- Page 219 and 220:
SYSTEMIC LUPUS ERYTHEMATOSUS (SLE)M
- Page 221 and 222:
VASCULITISLARGE-VESSEL VASCULITISTa
- Page 223 and 224:
Maintenance: MTX or AZA for 2 yfor
- Page 225 and 226:
CRYOGLOBULINEMIADefinition & Types
- Page 227 and 228:
CHANGE IN MENTAL STATUSDefinitions
- Page 229 and 230:
SEIZURESDefinitions (NEJM 2003;349:
- Page 231 and 232:
ALCOHOL WITHDRAWALPathophysiology
- Page 233 and 234:
Treatment of ischemic stroke (NEJM
- Page 235 and 236:
MYASTHENIA GRAVISDefinition and epi
- Page 237 and 238:
BACK AND SPINAL CORD DISEASEDdx of
- Page 239 and 240:
ACLS ALGORITHMSFigure 10-1 ACLS VF/
- Page 241 and 242:
Figure 10-3 ACLS bradycardia algori
- Page 243 and 244:
DrugClassDoseper kgaverageSedationM
- Page 245 and 246:
FORMULAE AND QUICK REFERENCECARDIOL
- Page 247 and 248:
P KUOsmFigure 10-5 Acetaminophen to
- Page 249 and 250:
Warfarin-heparin overlap therapy•
- Page 251 and 252:
5-NT6-MPa/wAAAAADAbABEABGabnlABPAab
- Page 253 and 254:
FRCFSGSFSHFTIFUOFVCG6PDGBGBMGBSGCAG
- Page 255 and 256:
PIDPIFPIPPKDPMPMFPMHxPMIPMLPMNPMVPM
- Page 257 and 258:
AA-a gradient, 2-18, 10-8abdominal
- Page 259 and 260:
Ddactylitis, 8-7decerebrate posturi
- Page 261 and 262:
Liddle’s syndrome, 4-5, 4-10, 7-8
- Page 263 and 264:
shock, 1-13, 10-4cardiogenic, 1-13s
- Page 265 and 266:
NOTES
- Page 267 and 268:
RadiologyPHOTO INSERT P-11 Normal P
- Page 269 and 270:
PHOTO INSERT P-37 Right middle lobe
- Page 271 and 272:
13 Normal chest CT at level of pulm
- Page 273 and 274:
17 Normal abdomen CT at level of li
- Page 275 and 276:
EchocardiographyVentricular septumR
- Page 277 and 278:
Anterolateralfree wallLeft ventricl
- Page 279 and 280:
Coronary Angiography3LEFT CORONARY
- Page 281:
PHOTO INSERT P-153 CML. 4 CLL.All p