AF 1-36Strategies for recurrent AF• Rate control: goal HR typically 60–80 at rest (although no clear benefit vs. goal110, NEJM 2010;362:1363) and 90–115 w/ exertion (see above table for options)AV node ablation PPM as a last resort (NEJM 2001;344:1043; NEJM 2002;346:2062)• Rhythm control: no clear survival benefit vs. rate ctrl (NEJM 2002;347:1825 & 2008;358:2667)• Anticoag (if indicated) to prevent thromboemboli, whether rate or rhythm strategyAntiarrhythmic Drugs (AAD) for AFAgent Conversion Maintenance CommentsAmiodarone 5–7 mg/kg IV over 200–400 mg qd c QT but TdP rare30–60’ S 1 mg/min (most effective Pulm, liver, thyroid toxicityto achieve 10-g load drug) ✓ PFTs, LFTs,TFTsDronedarone n/a 400 mg bid c QT, contraindic severe CHFT side effects c/w amioT efficacy but also T CV mortIII Ibutilide 1 mg IV over 10’ n/a Contraindic. if T K or c QTmay repeat 1c QT, 3–8% risk of TdPMg 1–2 g IV to T risk TdPDofetilide 0.5 mg PO bid 0.5 mg bid c QT, c risk of TdPRenally adjust doseSotalol n/a 90–160 mg bid ✓ for T HR, c QTRenally adjust doseFlecainide 300 mg PO 1 100–150 mg bid PreRx w/ AVN blockerIC Propafenone 600 mg PO 1 150–300 mg tid Contraindic. if structural orischemic heart diseaseIAProcainamide 10–15 mg/kg IV 1–2 g bid of T BP; c QTover 1 h slow release PreRx w/ AVN blocker(JACC 2006;48:e149; NEJM 2007;357:987 & 2009;360:668; JACC 2009;54:1089)• Lone AF S class IC drugs or sotalol, ? statins• CAD S class III drugs• CHF S dofetilide or amiodarone (NEJM 2007;356:935)Cardioversion• Consider pharm or DC cardioversion w/ 1st AF episode of if sx;if AF 48 h, 2–5% risk stroke w/ cardioversion (pharm. or electric)∴ either TEE to r/o thrombus or therapeutic anticoagulation for 3 wks prior• Likelihood of success dependent on AF duration (better 7 d) and atrial size• Consider pre-Rx w/ antiarrhythmic drugs (especially if 1st attempt fails)• For pharmacologic cardioversion, class III and IC drugs have best proven efficacy• Even if SR returns, atria mechanically stunned.Also, greatest likelihood of recurrent AFin first 3 mos after return to SR, ∴ must anticoagulate postcardioversion 4–12 wks.• “Pill-in-pocket”: if IC drugs have been safely tolerated in Pts w/o ischemic orstructural heart disease, can take as outPt prn if recurrent sx AF (NEJM 2004;351:2384)Nonpharmacologic therapy• Radiofrequency ablation (circumferential pulm. vein isolation): 80% success; considerif T EF or AADs failed/contraindic (NEJM 2006;354:934; JAMA 2005;293:2634 & 2010;303:333)• Surgical “maze” procedure (70–95% success rate) option if undergoing cardiac surgery• Left atrial appendage closure if undergoing cardiac surgery T risk of stroke; percutaneo<strong>usc</strong>losure may be comparable to warfarin and w/ T risk of ICH (Lancet 2009;374:534)Anticoagulation (JACC 2006;48:e149; Chest 2008;133:546S)• Risk of stroke 4.5% per year in nonvalvular AF; risk factors include:CHADS 2: CHF (1 point), HTN (1), Age 75 y (1), DM (1), prior Stroke/TIA (2)echo: EF 35%, dense spontaneous echo contrast in LAA, ? c LA size, ? Ao athero• Risk of stroke cc in valvular AF, anticoagulate all• Rx options: warfarin (INR 2–3) S 68% T stroke (heparin S warfarin bridge if h/o stroke)ASA (81–325 mg/d): better than placebo (21% T stroke) but inferior to warfarinASAclopi inferior to warfarin but T stroke (& c bleed) c/w ASA alone (NEJM 2009;360:2066)? dabigatran (oral direct thrombin inhib): 100 mg bid ≈ efficacy & T bleeding and 150 mgbid T stroke and ≈ bleeding c/w warfarin (w/o need to ✓ INR; RE-LY, NEJM 2009;361:1139)• Whom to Rx: valvular AF, prior stroke/TIA, or 2 risk factors S warfarin1 risk factor S warfarin or ASA; 0 risk factors S ASAif not good candidate for warfarin (c risk of bleeding) S ASA ? clopidogrelif require ASAclopiwarfarin (eg,AF & s/p recent stenting): INR 2–2.5,ASA 75–81 mg/d
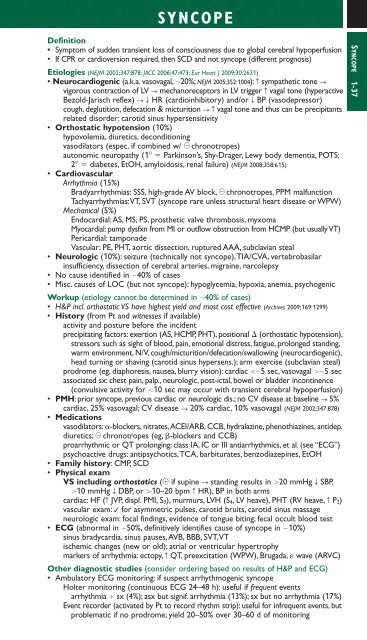
SYNCOPEDefinition• Symptom of sudden transient loss of consciousness due to global cerebral hypoperfusion• If CPR or cardioversion required, then SCD and not syncope (different prognosis)Etiologies (NEJM 2002;347:878; JACC 2006;47:473; Eur Heart J 2009;30:2631)• Neurocardiogenic (a.k.a. vasovagal, 20%; NEJM 2005;352:1004): c sympathetic tone Svigorous contraction of LV S mechanoreceptors in LV trigger c vagal tone (hyperactiveBezold-Jarisch reflex) STHR (cardioinhibitory) and/or T BP (vasodepressor)cough, deglutition, defecation & micturition Scvagal tone and thus can be precipitantsrelated disorder: carotid sinus hypersensitivity• Orthostatic hypotension (10%)hypovolemia, diuretics, deconditioningvasodilators (espec. if combined w/ chronotropes)autonomic neuropathy (1 Parkinson’s, Shy-Drager, Lewy body dementia, POTS;2 diabetes, EtOH, amyloidosis, renal failure) (NEJM 2008;358:615)• CardiovascularArrhythmia (15%)Bradyarrhythmias: SSS, high-grade AV block, chronotropes, PPM malfunctionTachyarrhythmias:VT, SVT (syncope rare unless structural heart disease or WPW)Mechanical (5%)Endocardial:AS, MS, PS, prosthetic valve thrombosis, myxomaMyocardial: pump dysfxn from MI or outflow obstruction from HCMP (but usually VT)Pericardial: tamponadeVascular: PE, PHT, aortic dissection, ruptured AAA, subclavian steal• Neurologic (10%): seizure (technically not syncope),TIA/CVA, vertebrobasilarinsufficiency, dissection of cerebral arteries, migraine, narcolepsy• No cause identified in 40% of cases• Misc. causes of LOC (but not syncope): hypoglycemia, hypoxia, anemia, psychogenicWorkup (etiology cannot be determined in 40% of cases)• H&P incl. orthostatic VS have highest yield and most cost effective (Archives 2009;169:1299)• History (from Pt and witnesses if available)activity and posture before the incidentprecipitating factors: exertion (AS, HCMP, PHT), positional (orthostatic hypotension),stressors such as sight of blood, pain, emotional distress, fatigue, prolonged standing,warm environment, N/V, cough/micturition/defecation/swallowing (neurocardiogenic),head turning or shaving (carotid sinus hypersens.); arm exercise (subclavian steal)prodrome (eg, diaphoresis, nausea, blurry vision): cardiac 5 sec, vasovagal 5 secassociated sx: chest pain, palp., neurologic, post-ictal, bowel or bladder incontinence(convulsive activity for 10 sec may occur with transient cerebral hypoperfusion)• PMH: prior syncope, previous cardiac or neurologic dis.; no CV disease at baseline S 5%cardiac, 25% vasovagal; CV disease S 20% cardiac, 10% vasovagal (NEJM 2002;347:878)• Medicationsvasodilators: -blockers, nitrates,ACEI/ARB, CCB, hydralazine, phenothiazines, antidep.diuretics; chronotropes (eg, -blockers and CCB)proarrhythmic or QT prolonging: class IA, IC or III antiarrhythmics, et al. (see “ECG”)psychoactive drugs: antipsychotics,TCA, barbiturates, benzodiazepines, EtOH• Family history: CMP, SCD• Physical examVS including orthostatics ( if supine S standing results in 20 mmHg T SBP,10 mmHg T DBP, or 10–20 bpm c HR), BP in both armscardiac: HF (c JVP, displ. PMI, S 3), murmurs, LVH (S 4, LV heave), PHT (RV heave, c P 2)vascular exam: ✓ for asymmetric pulses, carotid bruits, carotid sinus massageneurologic exam: focal findings, evidence of tongue biting; fecal occult blood test• ECG (abnormal in 50%, definitively identifies cause of syncope in 10%)sinus bradycardia, sinus pauses,AVB, BBB, SVT,VTischemic changes (new or old); atrial or ventricular hypertrophymarkers of arrhythmia: ectopy, c QT, preexcitation (WPW), Brugada, wave (ARVC)Other diagnostic studies (consider ordering based on results of H&P and ECG)• Ambulatory ECG monitoring: if suspect arrhythmogenic syncopeHolter monitoring (continuous ECG 24–48 h): useful if frequent eventsarrhythmia sx (4%); asx but signif. arrhythmia (13%); sx but no arrhythmia (17%)Event recorder (activated by Pt to record rhythm strip): useful for infrequent events, butproblematic if no prodrome; yield 20–50% over 30–60 d of monitoringSYNCOPE 1-37
- Page 3 and 4: POCKETNOTEBOOKPocketMEDICINEFourth
- Page 5 and 6: Contributing AuthorsForewordPreface
- Page 7 and 8: HIV/AIDS 6-17Tick-Borne Diseases 6-
- Page 9 and 10: Rajat Gupta, MDInternal Medicine Re
- Page 11 and 12: FOREWORDTo the 1st EditionIt is wit
- Page 13 and 14: ELECTROCARDIOGRAPHYApproach (a syst
- Page 15 and 16: CHEST PAINDisorderUnstableanginaMIP
- Page 17 and 18: CORONARY ANGIOGRAPHY AND REVASCULAR
- Page 19 and 20: Likelihood of ACSFeature High Inter
- Page 21 and 22: STEMIReperfusion• Immediate reper
- Page 23 and 24: • VT/VF: lido or amio 6-24 h, th
- Page 25 and 26: PA Catheter WaveformsLocation RA RV
- Page 27 and 28: Evaluation of the causes of heart f
- Page 29 and 30: CARDIOMYOPATHIESDiseases with mecha
- Page 31 and 32: RESTRICTIVE CARDIOMYOPATHY (RCMP)De
- Page 33 and 34: AORTIC INSUFFICIENCY (AI)Etiology (
- Page 35 and 36: Clinical manifestations (Lancet 200
- Page 37 and 38: PERICARDIAL DISEASEGENERAL PRINCIPL
- Page 39 and 40: CONSTRICTIVE PERICARDITISEtiology
- Page 41 and 42: • Pharmacologic options (if HTN o
- Page 43 and 44: ACUTE AORTIC SYNDROMESDefinitions (
- Page 45 and 46: OnsetRateRhythmP wavemorphologyResp
- Page 47: ATRIAL FIBRILLATIONClassification (
- Page 51 and 52: INTRACARDIAC DEVICESPacemaker CodeA
- Page 53 and 54: Pre-operative testing and therapy
- Page 55 and 56: DYSPNEAPathophysiologyEtiologiesAir
- Page 57 and 58: Other• Behavior modification: ide
- Page 59 and 60: CHRONIC OBSTRUCTIVE PULMONARY DISEA
- Page 61 and 62: HEMOPTYSISDefinition and pathophysi
- Page 63 and 64: INTERSTITIAL LUNG DISEASEWORKUP OF
- Page 65 and 66: PLEURAL EFFUSIONPathophysiology•
- Page 67 and 68: VENOUS THROMBOEMBOLISM (VTE)Definit
- Page 69 and 70: Risk stratification for Pts with PE
- Page 71 and 72: • SupportiveOxygen: maintain S aO
- Page 73 and 74: MECHANICAL VENTILATIONIndications
- Page 75 and 76: Tailoring the ventilator settings
- Page 77 and 78: SEPSISDefinitionsSystemic2 or more
- Page 79 and 80: ESOPHAGEAL AND GASTRIC DISORDERSDYS
- Page 81 and 82: GASTROINTESTINAL BLEEDINGDefinition
- Page 83 and 84: DIARRHEA, CONSTIPATION, AND ILEUSAC
- Page 85 and 86: Dx: IgA antitissue transglutaminase
- Page 87 and 88: DIVERTICULAR DISEASEDIVERTICULOSISD
- Page 89 and 90: MANAGEMENT (Lancet 2007;369:1641 &
- Page 91 and 92: PANCREATITISPathogenesis• Acinar
- Page 93 and 94: ABNORMAL LIVER TESTSTests of hepato
- Page 95 and 96: HEPATITISVIRALHepatitis A (ssRNA; a
- Page 97 and 98: AUTOIMMUNE HEPATITIS (AIH)Classific
- Page 99 and 100:
CIRRHOSISDefinition (Lancet 2008;37
- Page 101 and 102:
PrognosisModified Child-Turcotte-Pu
- Page 103 and 104:
HEPATIC VASCULAR DISEASEPortal vein
- Page 105 and 106:
BILIARY TRACT DISEASECHOLELITHIASIS
- Page 107 and 108:
ACID-BASE DISTURBANCESGENERALDefini
- Page 109 and 110:
Workup for AG metabolic acidosis•
- Page 111 and 112:
Etiologies of Metabolic AlkalosisSa
- Page 113 and 114:
Hypovolemic hypotonic hyponatremia
- Page 115 and 116:
POLYURIADefinition and pathophysiol
- Page 117 and 118:
Treatment• If true potassium defi
- Page 119 and 120:
Treatment• Treat underlying disor
- Page 121 and 122:
DIALYSISGeneral• Substitutes for
- Page 123 and 124:
Treatment• ANCA or anti-GBM: ste
- Page 125 and 126:
HEMATURIAEtiologies of HematuriaExt
- Page 127 and 128:
ANEMIAT in RBC mass: Hct 41% or Hb
- Page 129 and 130:
MACROCYTIC ANEMIASincludes megalobl
- Page 131 and 132:
• Infection: splenic infarction S
- Page 133 and 134:
PLATELET DISORDERSTHROMBOCYTOPENIA
- Page 135 and 136:
• Treatment of type II (NEJM 2006
- Page 137 and 138:
HYPERCOAGULABLE STATESSuspect in Pt
- Page 139 and 140:
TRANSFUSION THERAPYPacked red blood
- Page 141 and 142:
MYELOPROLIFERATIVE NEOPLASMS (MPN)G
- Page 143 and 144:
LEUKEMIAACUTE LEUKEMIADefinition•
- Page 145 and 146:
Prognosis• CR achieved in 80% of
- Page 147 and 148:
LYMPHOMADefinition• Malignant dis
- Page 149 and 150:
Consider CNS prophylaxis w/ intrath
- Page 151 and 152:
Treatment (NEJM 2004;351:1860; Lanc
- Page 153 and 154:
• Sinusoidal obstruction syndrome
- Page 155 and 156:
TNM Staging System for NSCLCN stage
- Page 157 and 158:
Simplified Staging System for Breas
- Page 159 and 160:
COLORECTAL CANCER (CRC)Epidemiology
- Page 161 and 162:
PANCREATIC TUMORSPathology and gene
- Page 163 and 164:
• Prostate, breast, and lung canc
- Page 165 and 166:
PNEUMONIAMicrobiology of PneumoniaC
- Page 167 and 168:
FUNGAL INFECTIONSCandida species•
- Page 169 and 170:
URINARY TRACT INFECTIONS (UTI)Defin
- Page 171 and 172:
Diagnostic studies• Superficial s
- Page 173 and 174:
INFECTIONS OF THE NERVOUS SYSTEMACU
- Page 175 and 176:
VIRAL ENCEPHALITISDefinition• Vir
- Page 177 and 178:
Diagnostic studies• Blood culture
- Page 179 and 180:
TUBERCULOSISEpidemiology• U.S.: 1
- Page 181 and 182:
HIV/AIDSDefinition• AIDS: HIV CD
- Page 183 and 184:
Cutaneous• Seborrheic dermatitis;
- Page 185 and 186:
TICK-BORNE DISEASESDistinguishing F
- Page 187 and 188:
FEVER OF UNKNOWN ORIGIN (FUO)Defini
- Page 189 and 190:
PITUITARY DISORDERSHYPOPITUITARY SY
- Page 191 and 192:
THYROID DISORDERSDiagnostic Studies
- Page 193 and 194:
Clinical manifestations of hyperthy
- Page 195 and 196:
ADRENAL DISORDERSCushing’s Syndro
- Page 197 and 198:
Treatment• Adenoma or carcinoma S
- Page 199 and 200:
CALCIUM DISORDERSLaboratory Finding
- Page 201 and 202:
DIABETES MELLITUSDefinition (Diabet
- Page 203 and 204:
Typical DKA “Flow sheet” SetupV
- Page 205 and 206:
ARTHRITIS—OVERVIEWApproach to pat
- Page 207 and 208:
RHEUMATOID ARTHRITIS (RA)Definition
- Page 209 and 210:
CRYSTAL DEPOSITION ARTHRITIDESGOUTD
- Page 211 and 212:
SERONEGATIVE SPONDYLOARTHRITISGENER
- Page 213 and 214:
INFECTIOUS ARTHRITIS & BURSITISDIAG
- Page 215 and 216:
CONNECTIVE TISSUE DISEASES% Autoant
- Page 217 and 218:
Clinical manifestations• Muscle w
- Page 219 and 220:
SYSTEMIC LUPUS ERYTHEMATOSUS (SLE)M
- Page 221 and 222:
VASCULITISLARGE-VESSEL VASCULITISTa
- Page 223 and 224:
Maintenance: MTX or AZA for 2 yfor
- Page 225 and 226:
CRYOGLOBULINEMIADefinition & Types
- Page 227 and 228:
CHANGE IN MENTAL STATUSDefinitions
- Page 229 and 230:
SEIZURESDefinitions (NEJM 2003;349:
- Page 231 and 232:
ALCOHOL WITHDRAWALPathophysiology
- Page 233 and 234:
Treatment of ischemic stroke (NEJM
- Page 235 and 236:
MYASTHENIA GRAVISDefinition and epi
- Page 237 and 238:
BACK AND SPINAL CORD DISEASEDdx of
- Page 239 and 240:
ACLS ALGORITHMSFigure 10-1 ACLS VF/
- Page 241 and 242:
Figure 10-3 ACLS bradycardia algori
- Page 243 and 244:
DrugClassDoseper kgaverageSedationM
- Page 245 and 246:
FORMULAE AND QUICK REFERENCECARDIOL
- Page 247 and 248:
P KUOsmFigure 10-5 Acetaminophen to
- Page 249 and 250:
Warfarin-heparin overlap therapy•
- Page 251 and 252:
5-NT6-MPa/wAAAAADAbABEABGabnlABPAab
- Page 253 and 254:
FRCFSGSFSHFTIFUOFVCG6PDGBGBMGBSGCAG
- Page 255 and 256:
PIDPIFPIPPKDPMPMFPMHxPMIPMLPMNPMVPM
- Page 257 and 258:
AA-a gradient, 2-18, 10-8abdominal
- Page 259 and 260:
Ddactylitis, 8-7decerebrate posturi
- Page 261 and 262:
Liddle’s syndrome, 4-5, 4-10, 7-8
- Page 263 and 264:
shock, 1-13, 10-4cardiogenic, 1-13s
- Page 265 and 266:
NOTES
- Page 267 and 268:
RadiologyPHOTO INSERT P-11 Normal P
- Page 269 and 270:
PHOTO INSERT P-37 Right middle lobe
- Page 271 and 272:
13 Normal chest CT at level of pulm
- Page 273 and 274:
17 Normal abdomen CT at level of li
- Page 275 and 276:
EchocardiographyVentricular septumR
- Page 277 and 278:
Anterolateralfree wallLeft ventricl
- Page 279 and 280:
Coronary Angiography3LEFT CORONARY
- Page 281:
PHOTO INSERT P-153 CML. 4 CLL.All p