url?sa=t&source=web&cd=2&ved=0CC0QFjAB&url=http://filletofish.net/usc/Pocket_Medicine_4th_Edition
url?sa=t&source=web&cd=2&ved=0CC0QFjAB&url=http://filletofish.net/usc/Pocket_Medicine_4th_Edition
url?sa=t&source=web&cd=2&ved=0CC0QFjAB&url=http://filletofish.net/usc/Pocket_Medicine_4th_Edition
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
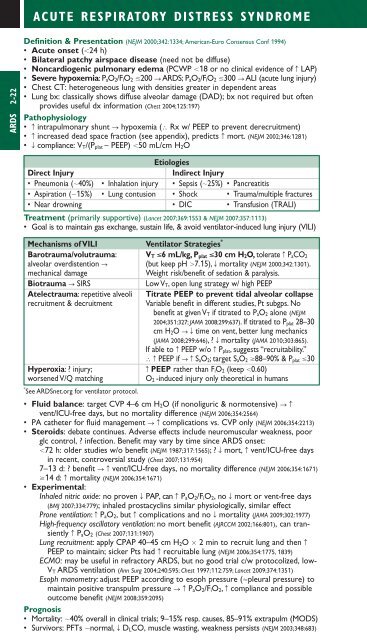
ACUTE RESPIRATORY DISTRESS SYNDROMEARDS 2-22Definition & Presentation (NEJM 2000;342:1334; American-Euro Consensus Conf 1994)• Acute onset (24 h)• Bilateral patchy airspace disease (need not be diffuse)• Noncardiogenic pulmonary edema (PCWP 18 or no clinical evidence of c LAP)• Severe hypoxemia: P aO 2/F iO 2 200 S ARDS; P aO 2/F iO 2 300 S ALI (acute lung injury)• Chest CT: heterogeneous lung with densities greater in dependent areas• Lung bx: classically shows diffuse alveolar damage (DAD); bx not required but oftenprovides useful dx information (Chest 2004;125:197)Pathophysiology• c intrapulmonary shunt S hypoxemia (∴ Rx w/ PEEP to prevent derecruitment)• c increased dead space fraction (see appendix), predicts c mort. (NEJM 2002;346:1281)• T compliance: V T/(P plat – PEEP) 50 mL/cm H 2OEtiologiesDirect InjuryIndirect Injury• Pneumonia (40%) • Inhalation injury • Sepsis (25%) • Pancreatitis• Aspiration (15%) • Lung contusion • Shock • Trauma/multiple fractures• Near drowning • DIC • Transfusion (TRALI)Treatment (primarily supportive) (Lancet 2007;369:1553 & NEJM 2007;357:1113)• Goal is to maintain gas exchange, sustain life, & avoid ventilator-induced lung injury (VILI)Mechanisms of VILI Ventilator Strategies *Barotrauma/volutrauma: V T 6 mL/kg, P plat 30 cm H 2O, tolerate c P aCO 2alveolar overdistention S (but keep pH 7.15), T mortality (NEJM 2000;342:1301).mechanical damageWeight risk/benefit of sedation & paralysis.Biotrauma S SIRSLow V T, open lung strategy w/ high PEEPAtelectrauma: repetitive alveoli Titrate PEEP to prevent tidal alveolar collapserecruitment & decruitment Variable benefit in different studies, Pt subgps. Nobenefit at given V T if titrated to P aO 2 alone (NEJM2004;351:327; JAMA 2008;299:637). If titrated to P plat 28–30cm H 2O STtime on vent, better lung mechanics(JAMA 2008;299:646),? T mortality (JAMA 2010;303:865).If able to c PEEP w/o c P plat, suggests “recruitability.”∴ c PEEP if ScS aO 2; target S aO 2 88–90% & P plat 30Hyperoxia: ? injury;c PEEP rather than F iO 2 (keep 0.60)worsened V/Q matchingO 2 -induced injury only theoretical in humans* See ARDS<strong>net</strong>.org for ventilator protocol.• Fluid balance: target CVP 4–6 cm H 2O (if nonoliguric & normotensive) S cvent/ICU-free days, but no mortality difference (NEJM 2006;354:2564)• PA catheter for fluid management S ccomplications vs. CVP only (NEJM 2006;354:2213)• Steroids: debate continues. Adverse effects include neurom<strong>usc</strong>ular weakness, poorglc control, ? infection. Benefit may vary by time since ARDS onset:72 h: older studies w/o benefit (NEJM 1987;317:1565); ? T mort, c vent/ICU-free daysin recent, controversial study (Chest 2007;131:954)7–13 d: ? benefit S cvent/ICU-free days, no mortality difference (NEJM 2006;354:1671)14 d: c mortality (NEJM 2006;354:1671)• Experimental:Inhaled nitric oxide: no proven T PAP, can c P aO 2/F iO 2, no T mort or vent-free days(BMJ 2007;334:779); inhaled prostacyclins similar physiologically, similar effectProne ventilation: c P aO 2, but c complications and no T mortality (JAMA 2009;302:1977)High-frequency oscillatory ventilation: no mort benefit (AJRCCM 2002;166:801), can transientlyc P aO 2 (Chest 2007;131:1907)Lung recruitment: apply CPAP 40–45 cm H 2O 2 min to recruit lung and then cPEEP to maintain; sicker Pts had c recruitable lung (NEJM 2006;354:1775, 1839)ECMO: may be useful in refractory ARDS, but no good trial c/w protocolized, low-V T ARDS ventilation (Ann Surg 2004;240:595; Chest 1997;112:759; Lancet 2009;374:1351)Esoph manometry: adjust PEEP according to esoph pressure (pleural pressure) tomaintain positive transpulm pressure S cP aO 2/F iO 2, c compliance and possibleoutcome benefit (NEJM 2008;359:2095)Prognosis• Mortality: 40% overall in clinical trials; 9–15% resp. causes, 85–91% extrapulm (MODS)• Survivors: PFTs normal, T D LCO, m<strong>usc</strong>le wasting, weakness persists (NEJM 2003;348:683)