url?sa=t&source=web&cd=2&ved=0CC0QFjAB&url=http://filletofish.net/usc/Pocket_Medicine_4th_Edition
url?sa=t&source=web&cd=2&ved=0CC0QFjAB&url=http://filletofish.net/usc/Pocket_Medicine_4th_Edition
url?sa=t&source=web&cd=2&ved=0CC0QFjAB&url=http://filletofish.net/usc/Pocket_Medicine_4th_Edition
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
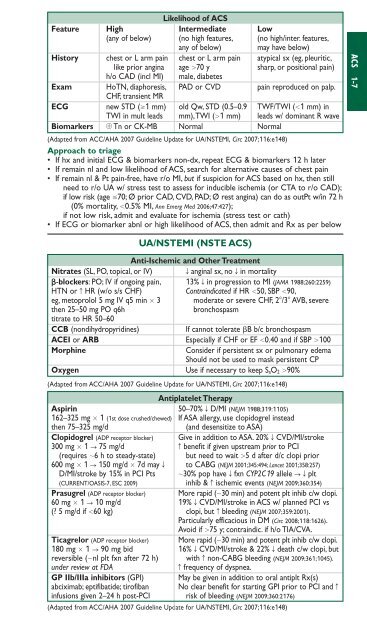
Likelihood of ACSFeature High Intermediate Low(any of below) (no high features, (no high/inter. features,any of below) may have below)History chest or L arm pain chest or L arm pain atypical sx (eg, pleuritic,like prior angina age 70 y sharp, or positional pain)h/o CAD (incl MI) male, diabetesExam HoTN, diaphoresis, PAD or CVD pain reproduced on palp.CHF, transient MRECG new STD (1 mm) old Qw, STD (0.5–0.9 TWF/TWI (1 mm) inTWI in mult leads mm),TWI (1 mm) leads w/ dominant R waveBiomarkers Tn or CK-MB Normal Normal(Adapted from ACC/AHA 2007 Guideline Update for UA/NSTEMI, Circ 2007;116:e148)Approach to triage• If hx and initial ECG & biomarkers non-dx, repeat ECG & biomarkers 12 h later• If remain nl and low likelihood of ACS, search for alternative causes of chest pain• If remain nl & Pt pain-free, have r/o MI, but if suspicion for ACS based on hx, then stillneed to r/o UA w/ stress test to assess for inducible ischemia (or CTA to r/o CAD);if low risk (age 70; Ø prior CAD, CVD, PAD; Ø rest angina) can do as outPt w/in 72 h(0% mortality, 0.5% MI, Ann Emerg Med 2006;47:427);if not low risk, admit and evaluate for ischemia (stress test or cath)• If ECG or biomarker abnl or high likelihood of ACS, then admit and Rx as per belowUA/NSTEMI (NSTE ACS)Anti-Ischemic and Other TreatmentNitrates (SL, PO, topical, or IV)T anginal sx, no T in mortality-blockers: PO; IV if ongoing pain, 13% T in progression to MI (JAMA 1988;260:2259)HTN or c HR (w/o s/s CHF) Contraindicated if HR 50, SBP 90,eg, metoprolol 5 mg IV q5 min 3 moderate or severe CHF, 2/3 AVB, severethen 25–50 mg PO q6hbronchospasmtitrate to HR 50–60CCB (nondihydropyridines)If cannot tolerate B b/c bronchospasmACEI or ARBEspecially if CHF or EF 0.40 and if SBP 100MorphineConsider if persistent sx or pulmonary edemaShould not be used to mask persistent CPOxygen Use if necessary to keep S aO 2 90%(Adapted from ACC/AHA 2007 Guideline Update for UA/NSTEMI, Circ 2007;116:e148)Antiplatelet TherapyAspirin 50–70% T D/MI (NEJM 1988;319:1105)162–325 mg 1 (1st dose crushed/chewed) If ASA allergy, use clopidogrel insteadthen 75–325 mg/d(and desensitize to ASA)Clopidogrel (ADP receptor blocker) Give in addition to ASA. 20% T CVD/MI/stroke300 mg 1 S 75 mg/d c benefit if given upstream prior to PCI(requires 6 h to steady-state) but need to wait 5 d after d/c clopi prior600 mg 1 S 150 mg/d 7d may T to CABG (NEJM 2001;345:494; Lancet 2001;358:257)D/MI/stroke by 15% in PCI Pts 30% pop have T fxn CYP2C19 allele STplt(CURRENT/OASIS-7, ESC 2009) inhib & c ischemic events (NEJM 2009;360:354)Prasugrel (ADP receptor blocker) More rapid (30 min) and potent plt inhib c/w clopi.60 mg 1 S 10 mg/d 19% T CVD/MI/stroke in ACS w/ planned PCI vs(? 5 mg/d if 60 kg) clopi, but c bleeding (NEJM 2007;359:2001).Particularly efficacious in DM (Circ 2008;118:1626).Avoid if 75 y; contraindic. if h/o TIA/CVA.Ticagrelor (ADP receptor blocker) More rapid (30 min) and potent plt inhib c/w clopi.180 mg 1 S 90 mg bid 16% T CVD/MI/stroke & 22% T death c/w clopi, butreversible (nl plt fxn after 72 h) with c non-CABG bleeding (NEJM 2009;361;1045).under review at FDAc frequency of dyspnea.GP IIb/IIIa inhibitors (GPI) May be given in addition to oral antiplt Rx(s)abciximab; eptifibatide; tirofiban No clear benefit for starting GPI prior to PCI and cinfusions given 2–24 h post-PCI risk of bleeding (NEJM 2009;360:2176)(Adapted from ACC/AHA 2007 Guideline Update for UA/NSTEMI, Circ 2007;116:e148)ACS 1-7