url?sa=t&source=web&cd=2&ved=0CC0QFjAB&url=http://filletofish.net/usc/Pocket_Medicine_4th_Edition
url?sa=t&source=web&cd=2&ved=0CC0QFjAB&url=http://filletofish.net/usc/Pocket_Medicine_4th_Edition
url?sa=t&source=web&cd=2&ved=0CC0QFjAB&url=http://filletofish.net/usc/Pocket_Medicine_4th_Edition
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
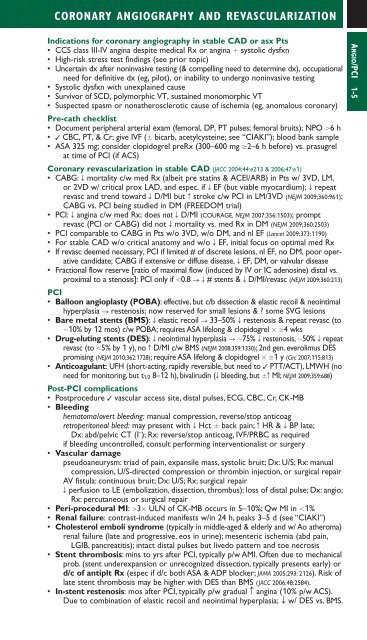
CORONARY ANGIOGRAPHY AND REVASCULARIZATIONIndications for coronary angiography in stable CAD or asx Pts• CCS class III-IV angina despite medical Rx or angina systolic dysfxn• High-risk stress test findings (see prior topic)• Uncertain dx after noninvasive testing (& compelling need to determine dx), occupationalneed for definitive dx (eg, pilot), or inability to undergo noninvasive testing• Systolic dysfxn with unexplained cause• Survivor of SCD, polymorphic VT, sustained monomorphic VT• Suspected spasm or nonatherosclerotic cause of ischemia (eg, anomalous coronary)Pre-cath checklist• Document peripheral arterial exam (femoral, DP, PT pulses; femoral bruits); NPO 6 h• ✓ CBC, PT, & Cr; give IVF ( bicarb, acetylcysteine; see “CIAKI”); blood bank sample• ASA 325 mg; consider clopidogrel preRx (300–600 mg 2–6 h before) vs. prasugrelat time of PCI (if ACS)Coronary revascularization in stable CAD (JACC 2004;44:e213 & 2006;47:e1)• CABG: T mortality c/w med Rx (albeit pre statins & ACEI/ARB) in Pts w/ 3VD, LM,or 2VD w/ critical prox LAD, and espec. if T EF (but viable myocardium); T repeatrevasc and trend toward T D/MI but c stroke c/w PCI in LM/3VD (NEJM 2009;360:961);CABG vs. PCI being studied in DM (FREEDOM trial)• PCI: T angina c/w med Rx; does not T D/MI (COURAGE, NEJM 2007;356:1503); promptrevasc (PCI or CABG) did not T mortality vs. med Rx in DM (NEJM 2009;360:2503)• PCI comparable to CABG in Pts w/o 3VD, w/o DM, and nl EF (Lancet 2009;373:1190)• For stable CAD w/o critical anatomy and w/o T EF, initial focus on optimal med Rx• If revasc deemed necessary, PCI if limited # of discrete lesions, nl EF, no DM, poor operativecandidate; CABG if extensive or diffuse disease, T EF, DM, or valvular disease• Fractional flow reserve [ratio of maximal flow (induced by IV or IC adenosine) distal vs.proximal to a stenosis]: PCI only if 0.8 ST# stents & T D/MI/revasc (NEJM 2009;360:213)PCI• Balloon angioplasty (POBA): effective, but c/b dissection & elastic recoil & neointimalhyperplasia S restenosis; now reserved for small lesions & ? some SVG lesions• Bare metal stents (BMS): T elastic recoil S 33–50% T restenosis & repeat revasc (to10% by 12 mos) c/w POBA; requires ASA lifelong & clopidogrel 4 wks• Drug-eluting stents (DES): T neointimal hyperplasia S 75% T restenosis, 50% T repeatrevasc (to 5% by 1 y), no c D/MI c/w BMS (NEJM 2008;359:1330); 2nd gen. everolimus DESpromising (NEJM 2010;362:1728); require ASA lifelong & clopidogrel 1 y (Circ 2007;115:813)• Anticoagulant: UFH (short-acting, rapidly reversible, but need to ✓ PTT/ACT), LMWH (noneed for monitoring, but t 1/2 8–12 h), bivalirudin (T bleeding, but c MI; NEJM 2009;359:688)Post-PCI complications• Postprocedure ✓ vascular access site, distal pulses, ECG, CBC, Cr, CK-MB• Bleedinghematoma/overt bleeding: manual compression, reverse/stop anticoagretroperitoneal bleed: may present with T Hct back pain; c HR & T BP late;Dx: abd/pelvic CT (I – ); Rx: reverse/stop anticoag, IVF/PRBC as requiredif bleeding uncontrolled, consult performing interventionalist or surgery• Vascular damagepseudoaneurysm: triad of pain, expansile mass, systolic bruit; Dx: U/S; Rx: manualcompression, U/S-directed compression or thrombin injection, or surgical repairAV fistula: continuous bruit; Dx: U/S; Rx: surgical repairT perfusion to LE (embolization, dissection, thrombus): loss of distal pulse; Dx: angio;Rx: percutaneous or surgical repair• Peri-procedural MI: 3 ULN of CK-MB occurs in 5–10%; Qw MI in 1%• Renal failure: contrast-induced manifests w/in 24 h, peaks 3–5 d (see “CIAKI”)• Cholesterol emboli syndrome (typically in middle-aged & elderly and w/ Ao atheroma)renal failure (late and progressive, eos in urine); mesenteric ischemia (abd pain,LGIB, pancreatitis); intact distal pulses but livedo pattern and toe necrosis• Stent thrombosis: mins to yrs after PCI, typically p/w AMI. Often due to mechanicalprob. (stent underexpansion or unrecognized dissection, typically presents early) ord/c of antiplt Rx (espec if d/c both ASA & ADP blocker; JAMA 2005;293: 2126). Risk oflate stent thrombosis may be higher with DES than BMS (JACC 2006;48:2584).• In-stent restenosis: mos after PCI, typically p/w gradual c angina (10% p/w ACS).Due to combination of elastic recoil and neointimal hyperplasia; T w/ DES vs. BMS.ANGIO/PCI 1-5