url?sa=t&source=web&cd=2&ved=0CC0QFjAB&url=http://filletofish.net/usc/Pocket_Medicine_4th_Edition
url?sa=t&source=web&cd=2&ved=0CC0QFjAB&url=http://filletofish.net/usc/Pocket_Medicine_4th_Edition
url?sa=t&source=web&cd=2&ved=0CC0QFjAB&url=http://filletofish.net/usc/Pocket_Medicine_4th_Edition
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
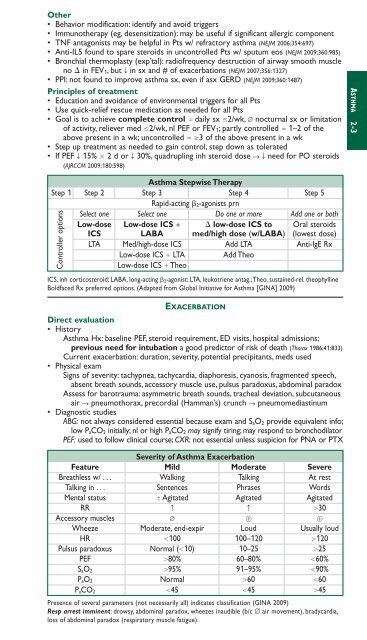
Other• Behavior modification: identify and avoid triggers• Immunotherapy (eg, desensitization): may be useful if significant allergic component• TNF antagonists may be helpful in Pts w/ refractory asthma (NEJM 2006;354:697)• Anti-IL5 found to spare steroids in uncontrolled Pts w/ sputum eos (NEJM 2009;360:985)• Bronchial thermoplasty (exp’tal): radiofrequency destruction of airway smooth m<strong>usc</strong>leno in FEV 1, but T in sx and # of exacerbations (NEJM 2007;356:1327)• PPI: not found to improve asthma sx, even if asx GERD (NEJM 2009;360:1487)Principles of treatment• Education and avoidance of environmental triggers for all Pts• Use quick-relief rescue medication as needed for all Pts• Goal is to achieve complete control daily sx 2/wk, ∅ nocturnal sx or limitationof activity, reliever med 2/wk, nl PEF or FEV 1; partly controlled 1–2 of theabove present in a wk; uncontrolled 3 of the above present in a wk• Step up treatment as needed to gain control, step down as tolerated• If PEF T 15% 2 d or T 30%, quadrupling inh steroid dose S Tneed for PO steroids(AJRCCM 2009;180:598)Asthma Stepwise TherapyStep 1 Step 2 Step 3 Step 4 Step 5Rapid-acting 2-agonists prnSelect one Select one Do one or more Add one or bothLow-dose Low-dose ICS low-dose ICS to Oral steroidsICS LABA med/high dose (w/LABA) (lowest dose)LTA Med/high-dose ICS Add LTA Anti-IgE RxLow-dose ICS LTA Add TheoLow-dose ICS TheoICS, inh corticosteroid; LABA, long-acting 2-agonist; LTA, leukotriene antag.;Theo, sustained-rel. theophyllineBoldfaced Rx preferred options. (Adapted from Global Initiative for Asthma [GINA] 2009)Controller optionsEXACERBATIONDirect evaluation• HistoryAsthma Hx: baseline PEF, steroid requirement, ED visits, hospital admissions;previous need for intubation a good predictor of risk of death (Thorax 1986;41:833)Current exacerbation: duration, severity, potential precipitants, meds used• Physical examSigns of severity: tachypnea, tachycardia, diaphoresis, cyanosis, fragmented speech,absent breath sounds, accessory m<strong>usc</strong>le use, pulsus paradoxus, abdominal paradoxAssess for barotrauma: asymmetric breath sounds, tracheal deviation, subcutaneousair S pneumothorax, precordial (Hamman’s) crunch S pneumomediastinum• Diagnostic studiesABG: not always considered essential because exam and S aO 2 provide equivalent info;low P aCO 2 initially; nl or high P aCO 2 may signify tiring; may respond to bronchodilatorPEF: used to follow clinical course; CXR: not essential unless suspicion for PNA or PTXSeverity of Asthma ExacerbationFeature Mild Moderate SevereBreathless w/ . . . Walking Talking At restTalking in . . . Sentences Phrases WordsMental status Agitated Agitated AgitatedRR c c 30Accessory m<strong>usc</strong>les ∅ Wheeze Moderate, end-expir Loud Usually loudHR 100 100–120 120Pulsus paradoxus Normal (10) 10–25 25PEF 80% 60–80% 60%S aO 2 95% 91–95% 90%P aO 2 Normal 60 60P aCO 2 45 45 45Presence of several parameters (not necessarily all) indicates classification (GINA 2009)Resp arrest imminent: drowsy, abdominal paradox, wheezes inaudible (b/c ∅ air movement), bradycardia,loss of abdominal paradox (respiratory m<strong>usc</strong>le fatigue).ASTHMA 2-3