Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
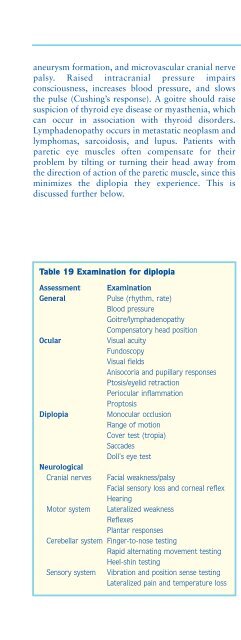
Disorders of special senses123aneurysm formation, and microvascular cranial nervepalsy. Raised intracranial pressure impairsconsciousness, increases blood pressure, and slowsthe pulse (Cushing’s response). A goitre should raisesuspicion of thyroid eye disease or myasthenia, whichcan occur in association with thyroid disorders.Lymphadenopathy occurs in metastatic neoplasm andlymphomas, sarcoidosis, and lupus. Patients withparetic eye muscles often compensate for theirproblem by tilting or turning their head away fromthe direction of action of the paretic muscle, since thisminimizes the diplopia they experience. This isdiscussed further below.Table 19 Examination for diplopiaAssessmentGeneralOcularDiplopiaNeurologicalCranial nervesMotor systemExaminationPulse (rhythm, rate)Blood pressureGoitre/lymphadenopathyCompensatory head positionVisual acuityFundoscopyVisual fieldsAnisocoria and pupillary responsesPtosis/eyelid retractionPeriocular inflammationProptosisMonocular occlusionRange of motionCover test (tropia)SaccadesDoll's eye testFacial weakness/palsyFacial sensory loss and corneal reflexHearingLateralized weaknessReflexesPlantar responsesCerebellar system Finger-to-nose testingRapid alternating movement testingHeel-shin testingSensory system Vibration and position sense testingLateralized pain and temperature lossOcular assessmentVisual fields, fundi and acuity should be assessed asdiscussed in the first section of this chapter. Pupillarysize, anisocoria (unequal pupils), and response tolight and accommodation are assessed. Pupillarydilatation can be subtle, and may not be fixed (inother words the response is sluggish and abnormal,but present). It occurs in (complete) third nervepalsies (because the third nerve carriesparasympathetic nerves which constrict the pupil),and should raise suspicion of a compressive aetiologybecause pupillary fibres lie superficially in the nervetrunk and are often affected first. Horner’s syndrome(a small pupil [miosis] more evident in the dark andptosis) indicates disruption of sympathetic nervesupply to the eye and, in the context of diplopia,raises suspicion of pathology at the cavernoussinus/superior orbital fissure or brainstem. Ptosis(drooping of the eyelid) should be looked for and thepalpebral aperture (distance between the eyelids)measured with a ruler to compare the two sides.Asking the patient to look upwards for 30 secondsbefore returning to the primary position andremeasuring assesses fatiguable ptosis. Cogan’s lidtwitch sign is a useful addition: the patient is asked tolook down for 10 seconds, and then quickly up to acentral target; the upper eyelid overshoots its normalposition and then comes down like a shutter to itsresting state. Fatiguable ptosis indicates a NMJdisorder, most commonly myasthenia. It is often, butnot exclusively, bilateral. It also occurs congenitallyand in chronic progressive external ophthalmoplegia.Unvarying ptosis may be due to mechanical disorders,a Horner’s syndrome (incomplete and with miosis) oroculomotor nerve palsy (typically more severe, andwith a normal or dilated pupil). Lid retraction occursin thyroid eye disease, in association with lid lag(lagging behind of the eyelid as it is shut). Proptosis isbest assessed by standing behind the patient andlooking downwards over the patient’s brows,comparing the positions of the two corneas relative toeach other and the superior orbital rims.Diplopia examinationA specific diplopia examination should also beperformed. Monocular occlusion is performedinitially, either looking straight ahead or in whicheverdirection the diplopia occurs, to determine whetherthis does abolish the double vision. For range ofmotion (duction testing) the patient is asked to a)look at the target, b) follow the target with their eyes