You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
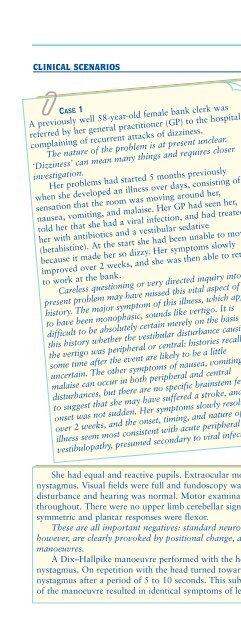
Disorders of special senses 143CLINICAL SCENARIOSCASE 1A previously well 58-year-old female bank clerk wasreferred by her general practitioner (GP) to the hospitalcomplaining of recurrent attacks of dizziness.The nature of the problem is at present unclear.‘Dizziness’ can mean many things and requires closerinvestigation.Her problems had started 5 months previouslywhen she developed an illness over days, consisting of asensation that the room was moving around her,nausea, vomiting, and malaise. Her GP had seen her,told her that she had a viral infection, and had treatedher with antibiotics and a vestibular sedative(betahistine). At the start she had been unable to movebecause it made her so dizzy. Her symptoms slowlyimproved over 2 weeks, and she was then able to returnto work at the bank.Careless questioning or very directed inquiry into thepresent problem may have missed this vital aspect of thehistory. The major symptom of this illness, which appearsto have been monophasic, sounds like vertigo. It isdifficult to be absolutely certain merely on the basis ofthis history whether the vestibular disturbance causingthe vertigo was peripheral or central: histories recalledsome time after the event are likely to be a littleuncertain. The other symptoms of nausea, vomiting, andmalaise can occur in both peripheral and centraldisturbances, but there are no specific brainstem featuresto suggest that she may have suffered a stroke, and theonset was not sudden. Her symptoms slowly resolvedover 2 weeks, and the onset, timing, and nature of theillness seem most consistent with acute peripheralvestibulopathy, presumed secondary to viral infection.Since that time she complained of recurringattacks of the room spinning around her in ahorizontal (yaw) plane. This was happening onmultiple occasions every day. Each attack lastedabout 10 seconds and seemed to occur whenevershe turned in bed, lay down, or sat up from thesupine position.This disorder is episodic, and the complaintis specifically one of vertigo. The problem isclearly positional, which immediately narrowsthe possibilities (for example cardiacarrhythmias are unlikely to be positional). Itdoes not appear to be a postural problem(suggesting postural hypotension), becauseturning and lying down cause difficulties asmuch as standing up. The duration of eachepisode is extremely short, and this is verycharacteristic of BPPV. It can also occur investibular decompensation after acute events.There were no other associatedsymptoms, including no visual symptoms, nonumbness, and no weakness. Her generalhealth was excellent in the past. She was ateetotal nonsmoker who exercised regularlyand lived with her husband. She was takingno medication when seen.These are important negatives: centraldisorders affecting vestibular tracts usually(but not always) cause other brainstemsymptoms. The lack of past history andlow vascular risk again make strokeunlikely as the cause of her initial illness.She had equal and reactive pupils. Extraocular movements were full and there was no spontaneousnystagmus. Visual fields were full and fundoscopy was normal. There was no facial weakness or sensorydisturbance and hearing was normal. Motor examination showed normal bulk, tone, and powerthroughout. There were no upper limb cerebellar signs and tandem gait was normal. Reflexes weresymmetric and plantar responses were flexor.These are all important negatives: standard neurological examination was normal. The symptoms,however, are clearly provoked by positional change, and so it is mandatory to perform positionalmanoeuvres.A Dix–Hallpike manoeuvre performed with the head turned toward the right did not produce anynystagmus. On repetition with the head turned toward the left, she developed an up-beating torsionalnystagmus after a period of 5 to 10 seconds. This subsided after an additional 10–15 seconds. Repetitionof the manoeuvre resulted in identical symptoms of lesser severity. (Continued overleaf)