magazine-pdf.org_13325_Better_Nutrition_April_2017_2
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
#$%&'()*+,-./*+0<br />
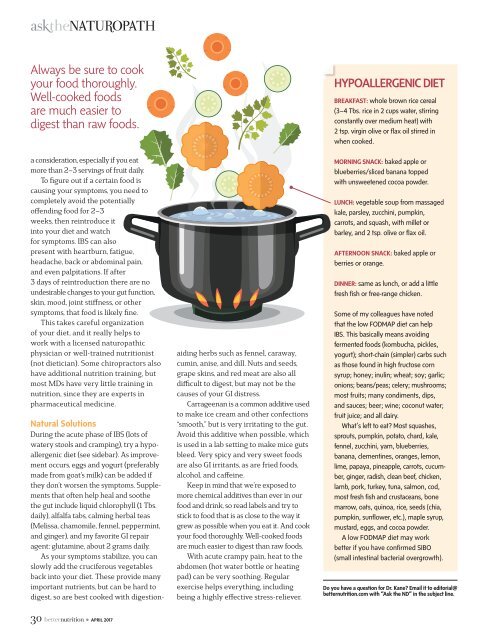
Always be sure to cook<br />
your food thoroughly.<br />
Well-cooked foods<br />
are much easier to<br />
digest than raw foods.<br />
a consideration, especially if you eat<br />
more than 2–3 servings of fruit daily.<br />
To figure out if a certain food is<br />
causing your symptoms, you need to<br />
completely avoid the potentially<br />
offending food for 2–3<br />
weeks, then reintroduce it<br />
into your diet and watch<br />
for symptoms. IBS can also<br />
present with heartburn, fatigue,<br />
headache, back or abdominal pain,<br />
and even palpitations. If after<br />
3 days of reintroduction there are no<br />
undesirable changes to your gut function,<br />
skin, mood, joint stiffness, or other<br />
symptoms, that food is likely fine.<br />
This takes careful <strong>org</strong>anization<br />
of your diet, and it really helps to<br />
work with a licensed naturopathic<br />
physician or well-trained nutritionist<br />
(not dietician). Some chiropractors also<br />
have additional nutrition training, but<br />
most MDs have very little training in<br />
nutrition, since they are experts in<br />
pharmaceutical medicine.<br />
Natural Solutions<br />
During the acute phase of IBS (lots of<br />
watery stools and cramping), try a hypoallergenic<br />
diet (see sidebar). As improvement<br />
occurs, eggs and yogurt (preferably<br />
made from goat’s milk) can be added if<br />
they don’t worsen the symptoms. Supplements<br />
that often help heal and soothe<br />
the gut include liquid chlorophyll (1 Tbs.<br />
daily), alfalfa tabs, calming herbal teas<br />
(Melissa, chamomile, fennel, peppermint,<br />
and ginger), and my favorite GI repair<br />
agent: glutamine, about 2 grams daily.<br />
As your symptoms stabilize, you can<br />
slowly add the cruciferous vegetables<br />
back into your diet. These provide many<br />
important nutrients, but can be hard to<br />
digest, so are best cooked with digestionaiding<br />
herbs such as fennel, caraway,<br />
cumin, anise, and dill. Nuts and seeds,<br />
grape skins, and red meat are also all<br />
difficult to digest, but may not be the<br />
causes of your GI distress.<br />
Carrageenan is a common additive used<br />
to make ice cream and other confections<br />
“smooth,” but is very irritating to the gut.<br />
Avoid this additive when possible, which<br />
is used in a lab setting to make mice guts<br />
bleed. Very spicy and very sweet foods<br />
are also GI irritants, as are fried foods,<br />
alcohol, and caffeine.<br />
Keep in mind that we’re exposed to<br />
more chemical additives than ever in our<br />
food and drink, so read labels and try to<br />
stick to food that is as close to the way it<br />
grew as possible when you eat it. And cook<br />
your food thoroughly. Well-cooked foods<br />
are much easier to digest than raw foods.<br />
With acute crampy pain, heat to the<br />
abdomen (hot water bottle or heating<br />
pad) can be very soothing. Regular<br />
exercise helps everything, including<br />
being a highly effective stress-reliever.<br />
HYPOALLERGENIC DIET<br />
BREAKFAST: whole brown rice cereal<br />
(3–4 Tbs. rice in 2 cups water, stirring<br />
constantly over medium heat) with<br />
2 tsp. virgin olive or flax oil stirred in<br />
when cooked.<br />
MORNING SNACK: baked apple or<br />
blueberries/sliced banana topped<br />
with unsweetened cocoa powder.<br />
LUNCH: vegetable soup from massaged<br />
kale, parsley, zucchini, pumpkin,<br />
carrots, and squash, with millet or<br />
barley, and 2 tsp. olive or flax oil.<br />
AFTERNOON SNACK: baked apple or<br />
berries or orange.<br />
DINNER: same as lunch, or add a little<br />
fresh fish or free-range chicken.<br />
Some of my colleagues have noted<br />
that the low FODMAP diet can help<br />
IBS. This basically means avoiding<br />
fermented foods (kombucha, pickles,<br />
yogurt); short-chain (simpler) carbs such<br />
as those found in high fructose corn<br />
syrup; honey; inulin; wheat; soy; garlic;<br />
onions; beans/peas; celery; mushrooms;<br />
most fruits; many condiments, dips,<br />
and sauces; beer; wine; coconut water;<br />
fruit juice; and all dairy.<br />
What’s left to eat? Most squashes,<br />
sprouts, pumpkin, potato, chard, kale,<br />
fennel, zucchini, yam, blueberries,<br />
banana, clementines, oranges, lemon,<br />
lime, papaya, pineapple, carrots, cucumber,<br />
ginger, radish, clean beef, chicken,<br />
lamb, pork, turkey, tuna, salmon, cod,<br />
most fresh fish and crustaceans, bone<br />
marrow, oats, quinoa, rice, seeds (chia,<br />
pumpkin, sunflower, etc.), maple syrup,<br />
mustard, eggs, and cocoa powder.<br />
A low FODMAP diet may work<br />
better if you have confirmed SIBO<br />
(small intestinal bacterial overgrowth).<br />
Do you have a question for Dr. Kane? Email it to editorial@<br />
betternutrition.com with “Ask the ND” in the subject line.<br />
!" • APRIL <strong>2017</strong>