Dental Asia January/February 2019
For more than two decades, Dental Asia is the premium journal in linking dental innovators and manufacturers to its rightful audience. We devote ourselves in showcasing the latest dental technology and share evidence-based clinical philosophies to serve as an educational platform to dental professionals. Our combined portfolio of print and digital media also allows us to reach a wider market and secure our position as the leading dental media in the Asia Pacific region while facilitating global interactions among our readers.
For more than two decades, Dental Asia is the premium journal in linking dental innovators
and manufacturers to its rightful audience. We devote ourselves in showcasing the latest dental technology and share evidence-based clinical philosophies to serve as an educational platform to dental professionals. Our combined portfolio of print and digital media also allows us to reach a wider market and secure our position as the leading dental media in the Asia Pacific region while facilitating global interactions among our readers.
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>Dental</strong> Managment<br />
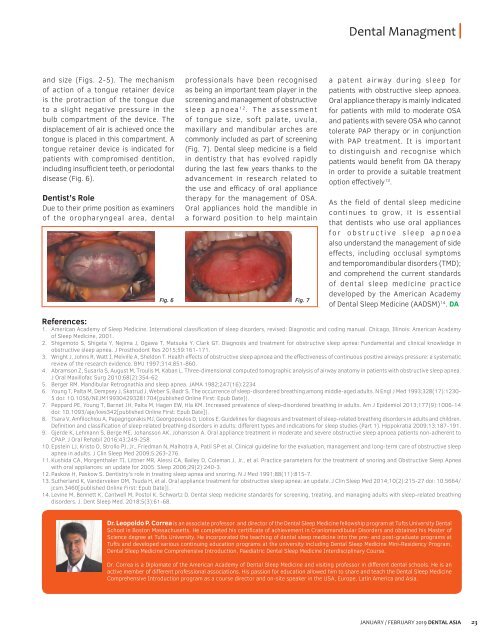
and size (Figs. 2-5). The mechanism<br />
of action of a tongue retainer device<br />
is the protraction of the tongue due<br />
to a slight negative pressure in the<br />
bulb compartment of the device. The<br />
displacement of air is achieved once the<br />
tongue is placed in this compartment. A<br />
tongue retainer device is indicated for<br />
patients with compromised dentition,<br />
including insufficient teeth, or periodontal<br />
disease (Fig. 6).<br />
Dentist’s Role<br />
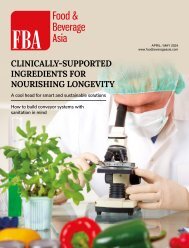
Due to their prime position as examiners<br />
of the oropharyngeal area, dental<br />
professionals have been recognised<br />
as being an important team player in the<br />
screening and management of obstructive<br />
sleep apnoea 12 . The assessment<br />
of tongue size, soft palate, uvula,<br />
maxillary and mandibular arches are<br />
commonly included as part of screening<br />
(Fig. 7). <strong>Dental</strong> sleep medicine is a field<br />
in dentistry that has evolved rapidly<br />
during the last few years thanks to the<br />
advancement in research related to<br />
the use and efficacy of oral appliance<br />
therapy for the management of OSA.<br />
Oral appliances hold the mandible in<br />
a forward position to help maintain<br />
Fig. 6 Fig. 7<br />
a patent airway during sleep for<br />
patients with obstructive sleep apnoea.<br />
Oral appliance therapy is mainly indicated<br />
for patients with mild to moderate OSA<br />
and patients with severe OSA who cannot<br />
tolerate PAP therapy or in conjunction<br />
with PAP treatment. It is important<br />
to distinguish and recognise which<br />
patients would benefit from OA therapy<br />
in order to provide a suitable treatment<br />
option effectively 13 .<br />
As the field of dental sleep medicine<br />
continues to grow, it is essential<br />
that dentists who use oral appliances<br />
for obstructive sleep apnoea<br />
also understand the management of side<br />
effects, including occlusal symptoms<br />
and temporomandibular disorders (TMD);<br />
and comprehend the current standards<br />
of dental sleep medicine practice<br />
developed by the American Academy<br />
of <strong>Dental</strong> Sleep Medicine (AADSM) 14 . DA<br />
References:<br />
1. American Academy of Sleep Medicine. International classification of sleep disorders, revised: Diagnostic and coding manual. Chicago, Illinois: American Academy<br />
of Sleep Medicine, 2001.<br />
2. Shigemoto S, Shigeta Y, Nejima J, Ogawa T, Matsuka Y, Clark GT. Diagnosis and treatment for obstructive sleep apnea: Fundamental and clinical knowledge in<br />
obstructive sleep apnea. J Prosthodont Res 2015;59:161-171.<br />
3. Wright J, Johns R, Watt I, Melville A, Sheldon T. Health effects of obstructive sleep apnoea and the effectiveness of continuous positive airways pressure: a systematic<br />
review of the research evidence. BMJ 1997;314:851-860.<br />
4. Abramson Z, Susarla S, August M, Troulis M, Kaban L. Three-dimensional computed tomographic analysis of airway anatomy in patients with obstructive sleep apnea.<br />
J Oral Maxillofac Surg 2010;68(2):354-62<br />
5. Berger RM. Mandibular Retrognathia and sleep apnea. JAMA 1982;247(16):2234<br />
6. Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med 1993;328(17):1230-<br />
5 doi: 10.1056/NEJM199304293281704[published Online First: Epub Date]|.<br />
7. Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol 2013;177(9):1006-14<br />
doi: 10.1093/aje/kws342[published Online First: Epub Date]|.<br />
8. Tsara V, Amfilochiou A, Papagrigorakis MJ, Georgopoulos D, Liolios E. Guidelines for diagnosis and treatment of sleep-related breathing disorders in adults and children.<br />
Definition and classification of sleep related breathing disorders in adults: different types and indications for sleep studies (Part 1). Hippokratia 2009;13:187-191.<br />
9. Gjerde K, Lehmann S, Berge ME, Johansson AK, Johansson A. Oral appliance treatment in moderate and severe obstructive sleep apnoea patients non-adherent to<br />
CPAP. J Oral Rehabil 2016;43:249-258.<br />
10. Epstein LJ, Kristo D, Strollo PJ, Jr., Friedman N, Malhotra A, Patil SP et al. Clinical guideline for the evaluation, management and long-term care of obstructive sleep<br />
apnea in adults. J Clin Sleep Med 2009;5:263-276.<br />
11. Kushida CA, Morgenthaler TI, Littner MR, Alessi CA, Bailey D, Coleman J, Jr., et al. Practice parameters for the treatment of snoring and Obstructive Sleep Apnea<br />
with oral appliances: an update for 2005. Sleep 2006;29(2):240-3.<br />
12. Paskow H, Paskow S. Dentistry’s role in treating sleep apnea and snoring. N J Med 1991;88(11):815-7.<br />
13. Sutherland K, Vanderveken OM, Tsuda H, et al. Oral appliance treatment for obstructive sleep apnea: an update. J Clin Sleep Med 2014;10(2):215-27 doi: 10.5664/<br />
jcsm.3460[published Online First: Epub Date]|.<br />
14. Levine M, Bennett K, Cantwell M, Postol K, Schwartz D. <strong>Dental</strong> sleep medicine standards for screening, treating, and managing adults with sleep-related breathing<br />
disorders. J. Dent Sleep Med. 2018;5(3):61-68.<br />
Dr. Leopoldo P. Correa is an associate professor and director of the <strong>Dental</strong> Sleep Medicine fellowship program at Tufts University <strong>Dental</strong><br />
School in Boston Massachusetts. He completed his certificate of achievement in Craniomandibular Disorders and obtained his Master of<br />
Science degree at Tufts University. He incorporated the teaching of dental sleep medicine into the pre- and post-graduate programs at<br />
Tufts and developed various continuing education programs at the university including <strong>Dental</strong> Sleep Medicine Mini-Residency Program,<br />
<strong>Dental</strong> Sleep Medicine Comprehensive Introduction, Paediatric <strong>Dental</strong> Sleep Medicine Interdisciplinary Course.<br />
Dr. Correa is a Diplomate of the American Academy of <strong>Dental</strong> Sleep Medicine and visiting professor in different dental schools. He is an<br />
active member of different professional associations. His passion for education allowed him to share and teach the <strong>Dental</strong> Sleep Medicine<br />
Comprehensive Introduction program as a course director and on-site speaker in the USA, Europe, Latin America and <strong>Asia</strong>.<br />
JANUARY / FEBRUARY <strong>2019</strong> DENTAL ASIA 23