Ch. 54 – Biliary System
Ch. 54 – Biliary System
Ch. 54 – Biliary System
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
1564 Section X Abdomen<br />
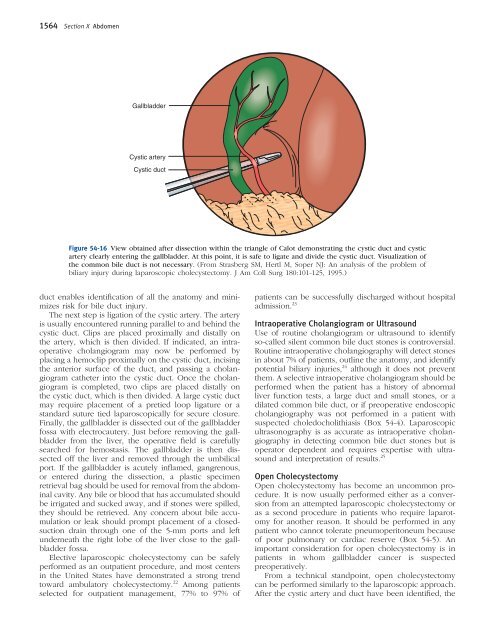
Gallbladder<br />
Cystic artery<br />
Cystic duct<br />
Figure <strong>54</strong>-16 View obtained after dissection within the triangle of Calot demonstrating the cystic duct and cystic<br />
artery clearly entering the gallbladder. At this point, it is safe to ligate and divide the cystic duct. Visualization of<br />
the common bile duct is not necessary. (From Strasberg SM, Hertl M, Soper NJ: An analysis of the problem of<br />
biliary injury during laparoscopic cholecystectomy. J Am Coll Surg 180:101-125, 1995.)<br />
duct enables identifi cation of all the anatomy and minimizes<br />
risk for bile duct injury.<br />
The next step is ligation of the cystic artery. The artery<br />
is usually encountered running parallel to and behind the<br />
cystic duct. Clips are placed proximally and distally on<br />
the artery, which is then divided. If indicated, an intraoperative<br />
cholangiogram may now be performed by<br />
placing a hemoclip proximally on the cystic duct, incising<br />
the anterior surface of the duct, and passing a cholangiogram<br />
catheter into the cystic duct. Once the cholangiogram<br />
is completed, two clips are placed distally on<br />
the cystic duct, which is then divided. A large cystic duct<br />
may require placement of a pretied loop ligature or a<br />
standard suture tied laparoscopically for secure closure.<br />
Finally, the gallbladder is dissected out of the gallbladder<br />
fossa with electrocautery. Just before removing the gallbladder<br />
from the liver, the operative fi eld is carefully<br />
searched for hemostasis. The gallbladder is then dissected<br />
off the liver and removed through the umbilical<br />
port. If the gallbladder is acutely infl amed, gangrenous,<br />
or entered during the dissection, a plastic specimen<br />
retrieval bag should be used for removal from the abdominal<br />
cavity. Any bile or blood that has accumulated should<br />
be irrigated and sucked away, and if stones were spilled,<br />
they should be retrieved. Any concern about bile accumulation<br />
or leak should prompt placement of a closedsuction<br />
drain through one of the 5-mm ports and left<br />
underneath the right lobe of the liver close to the gallbladder<br />
fossa.<br />
Elective laparoscopic cholecystectomy can be safely<br />
performed as an outpatient procedure, and most centers<br />
in the United States have demonstrated a strong trend<br />
toward ambulatory cholecystectomy. 22 Among patients<br />
selected for outpatient management, 77% to 97% of<br />
patients can be successfully discharged without hospital<br />
admission. 23<br />
Intraoperative <strong>Ch</strong>olangiogram or Ultrasound<br />
Use of routine cholangiogram or ultrasound to identify<br />
so-called silent common bile duct stones is controversial.<br />
Routine intraoperative cholangiography will detect stones<br />
in about 7% of patients, outline the anatomy, and identify<br />
potential biliary injuries, 24 although it does not prevent<br />
them. A selective intraoperative cholangiogram should be<br />
performed when the patient has a history of abnormal<br />
liver function tests, a large duct and small stones, or a<br />
dilated common bile duct, or if preoperative endoscopic<br />
cholangiography was not performed in a patient with<br />
suspected choledocholithiasis (Box <strong>54</strong>-4). Laparoscopic<br />
ultrasonography is as accurate as intraoperative cholangiography<br />
in detecting common bile duct stones but is<br />
operator dependent and requires expertise with ultrasound<br />
and interpretation of results. 25<br />
Open <strong>Ch</strong>olecystectomy<br />
Open cholecystectomy has become an uncommon procedure.<br />
It is now usually performed either as a conversion<br />
from an attempted laparoscopic cholecystectomy or<br />
as a second procedure in patients who require laparotomy<br />
for another reason. It should be performed in any<br />
patient who cannot tolerate pneumoperitoneum because<br />
of poor pulmonary or cardiac reserve (Box <strong>54</strong>-5). An<br />
important consideration for open cholecystectomy is in<br />
patients in whom gallbladder cancer is suspected<br />
preoperatively.<br />
From a technical standpoint, open cholecystectomy<br />
can be performed similarly to the laparoscopic approach.<br />
After the cystic artery and duct have been identifi ed, the