Ch. 54 – Biliary System
Ch. 54 – Biliary System
Ch. 54 – Biliary System
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
1574 Section X Abdomen<br />
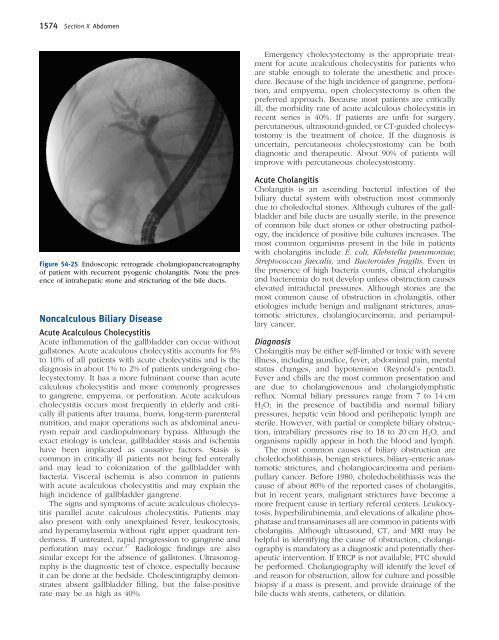
Figure <strong>54</strong>-25 Endoscopic retrograde cholangiopancreatography<br />
of patient with recurrent pyogenic cholangitis. Note the presence<br />
of intrahepatic stone and stricturing of the bile ducts.<br />
Noncalculous <strong>Biliary</strong> Disease<br />
Acute Acalculous <strong>Ch</strong>olecystitis<br />
Acute infl ammation of the gallbladder can occur without<br />
gallstones. Acute acalculous cholecystitis accounts for 5%<br />
to 10% of all patients with acute cholecystitis and is the<br />
diagnosis in about 1% to 2% of patients undergoing cholecystectomy.<br />
It has a more fulminant course than acute<br />
calculous cholecystitis and more commonly progresses<br />
to gangrene, empyema, or perforation. Acute acalculous<br />
cholecystitis occurs most frequently in elderly and critically<br />
ill patients after trauma, burns, long-term parenteral<br />
nutrition, and major operations such as abdominal aneurysm<br />
repair and cardiopulmonary bypass. Although the<br />
exact etiology is unclear, gallbladder stasis and ischemia<br />
have been implicated as causative factors. Stasis is<br />
common in critically ill patients not being fed enterally<br />
and may lead to colonization of the gallbladder with<br />
bacteria. Visceral ischemia is also common in patients<br />
with acute acalculous cholecystitis and may explain the<br />
high incidence of gallbladder gangrene.<br />
The signs and symptoms of acute acalculous cholecystitis<br />
parallel acute calculous cholecystitis. Patients may<br />
also present with only unexplained fever, leukocytosis,<br />
and hyperamylasemia without right upper quadrant tenderness.<br />
If untreated, rapid progression to gangrene and<br />
perforation may occur. 37 Radiologic fi ndings are also<br />
similar except for the absence of gallstones. Ultrasonography<br />
is the diagnostic test of choice, especially because<br />
it can be done at the bedside. <strong>Ch</strong>olescintigraphy demonstrates<br />
absent gallbladder fi lling, but the false-positive<br />
rate may be as high as 40%.<br />
Emergency cholecystectomy is the appropriate treatment<br />
for acute acalculous cholecystitis for patients who<br />
are stable enough to tolerate the anesthetic and procedure.<br />
Because of the high incidence of gangrene, perforation,<br />
and empyema, open cholecystectomy is often the<br />
preferred approach. Because most patients are critically<br />
ill, the morbidity rate of acute acalculous cholecystitis in<br />
recent series is 40%. If patients are unfi t for surgery,<br />
percutaneous, ultrasound-guided, or CT-guided cholecystostomy<br />
is the treatment of choice. If the diagnosis is<br />
uncertain, percutaneous cholecystostomy can be both<br />
diagnostic and therapeutic. About 90% of patients will<br />
improve with percutaneous cholecystostomy.<br />
Acute <strong>Ch</strong>olangitis<br />
<strong>Ch</strong>olangitis is an ascending bacterial infection of the<br />
biliary ductal system with obstruction most commonly<br />
due to choledochal stones. Although cultures of the gallbladder<br />
and bile ducts are usually sterile, in the presence<br />
of common bile duct stones or other obstructing pathology,<br />
the incidence of positive bile cultures increases. The<br />
most common organisms present in the bile in patients<br />
with cholangitis include E. coli, Klebsiella pneumoniae,<br />
Streptococcus faecalis, and Bacteroides fragilis. Even in<br />
the presence of high bacteria counts, clinical cholangitis<br />
and bacteremia do not develop unless obstruction causes<br />
elevated intraductal pressures. Although stones are the<br />
most common cause of obstruction in cholangitis, other<br />
etiologies include benign and malignant strictures, anastomotic<br />
strictures, cholangiocarcinoma, and periampullary<br />
cancer.<br />
Diagnosis<br />
<strong>Ch</strong>olangitis may be either self-limited or toxic with severe<br />
illness, including jaundice, fever, abdominal pain, mental<br />
status changes, and hypotension (Reynold’s pentad).<br />
Fever and chills are the most common presentation and<br />
are due to cholangiovenous and cholangiolymphatic<br />
refl ux. Normal biliary pressures range from 7 to 14 cm<br />
H 2O; in the presence of bactibilia and normal biliary<br />
pressures, hepatic vein blood and perihepatic lymph are<br />
sterile. However, with partial or complete biliary obstruction,<br />
intrabiliary pressures rise to 18 to 20 cm H 2O, and<br />
organisms rapidly appear in both the blood and lymph.<br />
The most common causes of biliary obstruction are<br />
choledocholithiasis, benign strictures, biliary-enteric anastomotic<br />
strictures, and cholangiocarcinoma and periampullary<br />
cancer. Before 1980, choledocholithiasis was the<br />
cause of about 80% of the reported cases of cholangitis,<br />
but in recent years, malignant strictures have become a<br />
more frequent cause in tertiary referral centers. Leukocytosis,<br />
hyperbilirubinemia, and elevations of alkaline phosphatase<br />
and transaminases all are common in patients with<br />
cholangitis. Although ultrasound, CT, and MRI may be<br />
helpful in identifying the cause of obstruction, cholangiography<br />
is mandatory as a diagnostic and potentially therapeutic<br />
intervention. If ERCP is not available, PTC should<br />
be performed. <strong>Ch</strong>olangiography will identify the level of<br />
and reason for obstruction, allow for culture and possible<br />
biopsy if a mass is present, and provide drainage of the<br />
bile ducts with stents, catheters, or dilation.