nr. 477 - 2011 - Institut for Natur, Systemer og Modeller (NSM)
nr. 477 - 2011 - Institut for Natur, Systemer og Modeller (NSM)
nr. 477 - 2011 - Institut for Natur, Systemer og Modeller (NSM)
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
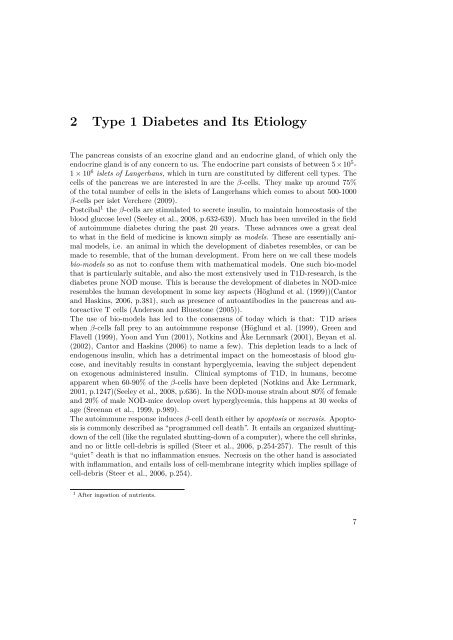
2 Type 1 Diabetes and Its Etiol<strong>og</strong>y<br />
The pancreas consists of an exocrine gland and an endocrine gland, of which only the<br />
endocrine gland is of any concern to us. The endocrine part consists of between 5×10 5 -<br />
1 × 10 6 islets of Langerhans, which in turn are constituted by different cell types. The<br />
cells of the pancreas we are interested in are the β-cells. They make up around 75%<br />
of the total number of cells in the islets of Langerhans which comes to about 500-1000<br />
β-cells per islet Verchere (2009).<br />
Postcibal 1 the β-cells are stimulated to secrete insulin, to maintain homeostasis of the<br />
blood glucose level (Seeley et al., 2008, p.632-639). Much has been unveiled in the field<br />
of autoimmune diabetes during the past 20 years. These advances owe a great deal<br />
to what in the field of medicine is known simply as models. These are essentially animal<br />
models, i.e. an animal in which the development of diabetes resembles, or can be<br />
made to resemble, that of the human development. From here on we call these models<br />
bio-models so as not to confuse them with mathematical models. One such bio-model<br />
that is particularly suitable, and also the most extensively used in T1D-research, is the<br />
diabetes prone NOD mouse. This is because the development of diabetes in NOD-mice<br />
resembles the human development in some key aspects (Höglund et al. (1999))(Cantor<br />
and Haskins, 2006, p.381), such as presence of autoantibodies in the pancreas and autoreactive<br />
T cells (Anderson and Bluestone (2005)).<br />
The use of bio-models has led to the consensus of today which is that: T1D arises<br />
when β-cells fall prey to an autoimmune response (Höglund et al. (1999), Green and<br />
Flavell (1999), Yoon and Yun (2001), Notkins and Åke Lernmark (2001), Beyan et al.<br />
(2002), Cantor and Haskins (2006) to name a few). This depletion leads to a lack of<br />
end<strong>og</strong>enous insulin, which has a detrimental impact on the homeostasis of blood glucose,<br />
and inevitably results in constant hyperglycemia, leaving the subject dependent<br />
on ex<strong>og</strong>enous administered insulin. Clinical symptoms of T1D, in humans, become<br />
apparent when 60-90% of the β-cells have been depleted (Notkins and Åke Lernmark,<br />
2001, p.1247)(Seeley et al., 2008, p.636). In the NOD-mouse strain about 80% of female<br />
and 20% of male NOD-mice develop overt hyperglycemia, this happens at 30 weeks of<br />
age (Sreenan et al., 1999, p.989).<br />
The autoimmune response induces β-cell death either by apoptosis or necrosis. Apoptosis<br />
is commonly described as “pr<strong>og</strong>rammed cell death”. It entails an organized shuttingdown<br />
of the cell (like the regulated shutting-down of a computer), where the cell shrinks,<br />
and no or little cell-debris is spilled (Steer et al., 2006, p.254-257). The result of this<br />
“quiet” death is that no inflammation ensues. Necrosis on the other hand is associated<br />
with inflammation, and entails loss of cell-membrane integrity which implies spillage of<br />
cell-debris (Steer et al., 2006, p.254).<br />
1 After ingestion of nutrients.<br />
7