NHMRC Glaucoma Guidelines - ANZGIG
NHMRC Glaucoma Guidelines - ANZGIG
NHMRC Glaucoma Guidelines - ANZGIG
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
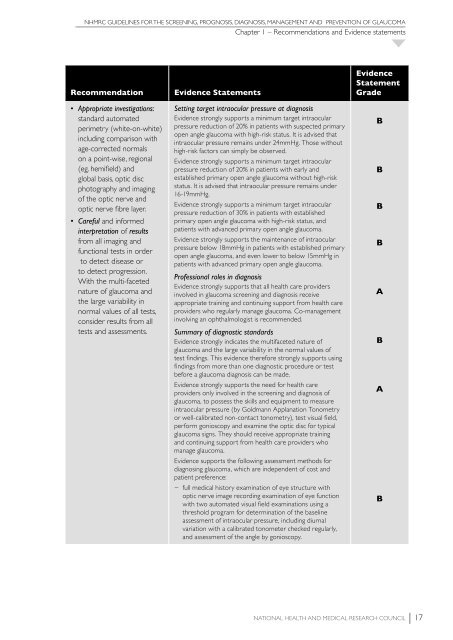
<strong>NHMRC</strong> GUIDELINES FOR THE SCREENING, PROGNOSIS, DIAGNOSIS, MANAGEMENT AND PREVENTION OF GLAUCOMA<br />
Chapter 1 – Recommendations and Evidence statements<br />
Recommendation<br />
• Appropriate investigations:<br />
standard automated<br />
perimetry (white-on-white)<br />
including comparison with<br />
age-corrected normals<br />
on a point-wise, regional<br />
(eg. hemifield) and<br />
global basis, optic disc<br />
photography and imaging<br />
of the optic nerve and<br />
optic nerve fibre layer.<br />
• Careful and informed<br />
interpretation of results<br />
from all imaging and<br />
functional tests in order<br />
to detect disease or<br />
to detect progression.<br />
With the multi-faceted<br />
nature of glaucoma and<br />
the large variability in<br />
normal values of all tests,<br />
consider results from all<br />
tests and assessments.<br />
Evidence Statements<br />
Setting target intraocular pressure at diagnosis<br />
Evidence strongly supports a minimum target intraocular<br />
pressure reduction of 20% in patients with suspected primary<br />
open angle glaucoma with high-risk status. It is advised that<br />
intraocular pressure remains under 24mmHg. Those without<br />
high-risk factors can simply be observed.<br />
Evidence strongly supports a minimum target intraocular<br />
pressure reduction of 20% in patients with early and<br />
established primary open angle glaucoma without high-risk<br />
status. It is advised that intraocular pressure remains under<br />
16-19mmHg.<br />
Evidence strongly supports a minimum target intraocular<br />
pressure reduction of 30% in patients with established<br />
primary open angle glaucoma with high-risk status, and<br />
patients with advanced primary open angle glaucoma.<br />
Evidence strongly supports the maintenance of intraocular<br />
pressure below 18mmHg in patients with established primary<br />
open angle glaucoma, and even lower to below 15mmHg in<br />
patients with advanced primary open angle glaucoma.<br />
Professional roles in diagnosis<br />
Evidence strongly supports that all health care providers<br />
involved in glaucoma screening and diagnosis receive<br />
appropriate training and continuing support from health care<br />
providers who regularly manage glaucoma. Co-management<br />
involving an ophthalmologist is recommended.<br />
Summary of diagnostic standards<br />
Evidence strongly indicates the multifaceted nature of<br />
glaucoma and the large variability in the normal values of<br />
test findings. This evidence therefore strongly supports using<br />
findings from more than one diagnostic procedure or test<br />
before a glaucoma diagnosis can be made.<br />
Evidence strongly supports the need for health care<br />
providers only involved in the screening and diagnosis of<br />
glaucoma, to possess the skills and equipment to measure<br />
intraocular pressure (by Goldmann Applanation Tonometry<br />
or well-calibrated non-contact tonometry), test visual field,<br />
perform gonioscopy and examine the optic disc for typical<br />
glaucoma signs. They should receive appropriate training<br />
and continuing support from health care providers who<br />
manage glaucoma.<br />
Evidence supports the following assessment methods for<br />
diagnosing glaucoma, which are independent of cost and<br />
patient preference:<br />
−−<br />
full medical history examination of eye structure with<br />
optic nerve image recording examination of eye function<br />
with two automated visual field examinations using a<br />
threshold program for determination of the baseline<br />
assessment of intraocular pressure, including diurnal<br />
variation with a calibrated tonometer checked regularly,<br />
and assessment of the angle by gonioscopy.<br />
Evidence<br />
Statement<br />
Grade<br />
B<br />
B<br />
B<br />
B<br />
A<br />
B<br />
A<br />
B<br />
National Health and Medical Research Council 17