Program Manual - Saint Louis University
Program Manual - Saint Louis University
Program Manual - Saint Louis University
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
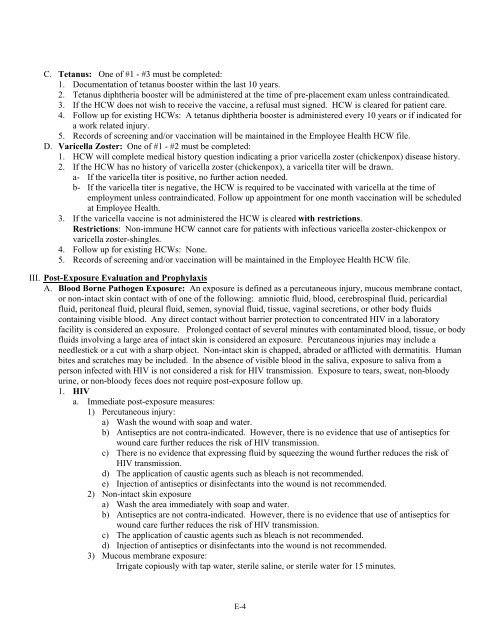
C. Tetanus: One of #1 - #3 must be completed:<br />
1. Documentation of tetanus booster within the last 10 years.<br />
2. Tetanus diphtheria booster will be administered at the time of pre-placement exam unless contraindicated.<br />
3. If the HCW does not wish to receive the vaccine, a refusal must signed. HCW is cleared for patient care.<br />
4. Follow up for existing HCWs: A tetanus diphtheria booster is administered every 10 years or if indicated for<br />
a work related injury.<br />
5. Records of screening and/or vaccination will be maintained in the Employee Health HCW file.<br />
D. Varicella Zoster: One of #1 - #2 must be completed:<br />
1. HCW will complete medical history question indicating a prior varicella zoster (chickenpox) disease history.<br />
2. If the HCW has no history of varicella zoster (chickenpox), a varicella titer will be drawn.<br />
a- If the varicella titer is positive, no further action needed.<br />
b- If the varicella titer is negative, the HCW is required to be vaccinated with varicella at the time of<br />
employment unless contraindicated. Follow up appointment for one month vaccination will be scheduled<br />
at Employee Health.<br />
3. If the varicella vaccine is not administered the HCW is cleared with restrictions.<br />
Restrictions: Non-immune HCW cannot care for patients with infectious varicella zoster-chickenpox or<br />
varicella zoster-shingles.<br />
4. Follow up for existing HCWs: None.<br />
5. Records of screening and/or vaccination will be maintained in the Employee Health HCW file.<br />
III. Post-Exposure Evaluation and Prophylaxis<br />
A. Blood Borne Pathogen Exposure: An exposure is defined as a percutaneous injury, mucous membrane contact,<br />
or non-intact skin contact with of one of the following: amniotic fluid, blood, cerebrospinal fluid, pericardial<br />
fluid, peritoneal fluid, pleural fluid, semen, synovial fluid, tissue, vaginal secretions, or other body fluids<br />
containing visible blood. Any direct contact without barrier protection to concentrated HIV in a laboratory<br />
facility is considered an exposure. Prolonged contact of several minutes with contaminated blood, tissue, or body<br />
fluids involving a large area of intact skin is considered an exposure. Percutaneous injuries may include a<br />
needlestick or a cut with a sharp object. Non-intact skin is chapped, abraded or afflicted with dermatitis. Human<br />
bites and scratches may be included. In the absence of visible blood in the saliva, exposure to saliva from a<br />
person infected with HIV is not considered a risk for HIV transmission. Exposure to tears, sweat, non-bloody<br />
urine, or non-bloody feces does not require post-exposure follow up.<br />
1. HIV<br />
a. Immediate post-exposure measures:<br />
1) Percutaneous injury:<br />
a) Wash the wound with soap and water.<br />
b) Antiseptics are not contra-indicated. However, there is no evidence that use of antiseptics for<br />
wound care further reduces the risk of HIV transmission.<br />
c) There is no evidence that expressing fluid by squeezing the wound further reduces the risk of<br />
HIV transmission.<br />
d) The application of caustic agents such as bleach is not recommended.<br />
e) Injection of antiseptics or disinfectants into the wound is not recommended.<br />
2) Non-intact skin exposure<br />
a) Wash the area immediately with soap and water.<br />
b) Antiseptics are not contra-indicated. However, there is no evidence that use of antiseptics for<br />
wound care further reduces the risk of HIV transmission.<br />
c) The application of caustic agents such as bleach is not recommended.<br />
d) Injection of antiseptics or disinfectants into the wound is not recommended.<br />
3) Mucous membrane exposure:<br />
Irrigate copiously with tap water, sterile saline, or sterile water for 15 minutes.<br />
E-4