- Page 1 and 2:
Adult Medical Emergencies EDITOR Dr
- Page 3 and 4:
WGH IN CARDIAC ARREST & LIFE THREAT
- Page 5 and 6:
RIE USEFUL BLEEP NUMBERS MED REG (w
- Page 7 and 8:
ST JOHN’S THEATRES 1-9 1 ........
- Page 9 and 10:
OTHER USEFUL TELEPHONE NUMBERS NAME
- Page 11 and 12:
Management of First Seizure in Adul
- Page 13 and 14:
Addison’s Disease ...............
- Page 15 and 16:
EDITOR’S INTRODUCTION The Adult M
- Page 17 and 18:
DISCLAIMER Every effort has been ma
- Page 19 and 20:
GENERAL POINTS Medicines • Doses
- Page 21 and 22:
i as far as is reasonably possible.
- Page 23 and 24:
i GOOD DOCUMENTATION • Write legi
- Page 25 and 26:
• Prescribe liquids by writing th
- Page 27 and 28:
Figure 1 Figure 2 Figure 3 Figure 4
- Page 29 and 30:
MAKING A DECISION ABOUT RESUSCITATI
- Page 31 and 32:
THE PATIENT WHO IS NOT COMPETENT TO
- Page 33 and 34:
i PATIENT DEATHS • See patients w
- Page 35 and 36:
CHECKLIST OF REQUIREMENTS This chec
- Page 37 and 38:
ORGAN DONATION Transplants are one
- Page 39 and 40:
i Always consider telephoning the G
- Page 41 and 42:
i review arrangements. Include: a)
- Page 43 and 44:
Immediate investigations are those
- Page 45 and 46:
i i NOTES ON INITIAL ASSESSMENT ALG
- Page 47 and 48:
i Exposure, evidence and examinatio
- Page 49 and 50:
i i 2b. ILLNESS SEVERITY ASSESSMENT
- Page 51 and 52:
Observation Chart Date chart commen
- Page 53 and 54:
i Illness Severity and Diagnosis (R
- Page 55 and 56:
i Watch for the development of card
- Page 57 and 58:
SHOCK Definition & Classification
- Page 59 and 60: i Cuff BP by machine may be extreme
- Page 61 and 62: If no bleeding and platelets
- Page 63 and 64: TRANSFUSION REACTION Figure 1: Algo
- Page 65 and 66: of infusing only 5-10mls of blood.
- Page 67 and 68: Table 3: Drugs that may be required
- Page 69 and 70: i i SEPSIS AND SEPTIC SHOCK Sepsis
- Page 71 and 72: ANTIBIOTIC MINI-GUIDE FOR ADULTS
- Page 73 and 74: i i • Remember to look for intra-
- Page 75 and 76: i • Commence basic life support (
- Page 77 and 78: ALGORITHM FOR FIRST MEDICAL RESPOND
- Page 79 and 80: ACUTE PAIN MANAGEMENT The effective
- Page 81 and 82: i DO YOU NEED HELP ? Contact the Ac
- Page 83 and 84: i • Angina (rate related): treat
- Page 85 and 86: DATE: Dear “FIRST SEIZURE” APPO
- Page 87 and 88: Review Collapse Algorithm Identifie
- Page 89 and 90: Loss of consciousness YES Perform:
- Page 91 and 92: 07.00 to 17.00 Asymptomatic Normal
- Page 93 and 94: i i ADULT ADVANCED LIFE SUPPORT: No
- Page 95 and 96: i NON SHOCKABLE RHYTHMS Cardiac arr
- Page 97 and 98: • Patients should be pain free an
- Page 99 and 100: ACUTE CORONARY SYNDROMES In order t
- Page 101 and 102: IMMEDIATE MANAGEMENT OF ACUTE CORON
- Page 103 and 104: CHEST PAIN PATHWAY - NHS LOTHIAN OP
- Page 105 and 106: LOTHIAN PRIMARY PCI/PRE-HOSPITAL TH
- Page 107 and 108: i Thrombolysis Since the clinical b
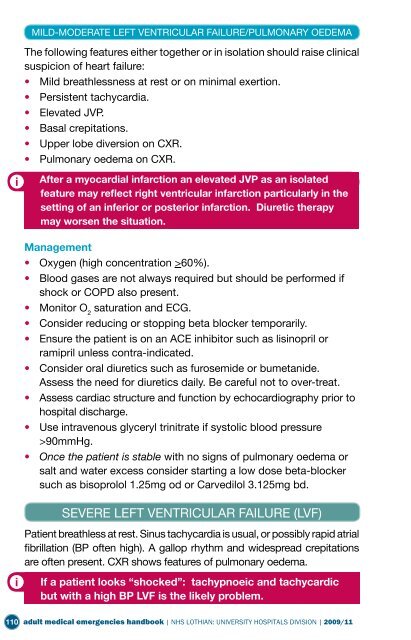
- Page 109: Reperfusion therapy not administere
- Page 113 and 114: i i Do not hesitate to seek a Cardi
- Page 115 and 116: account any subsequently prescribed
- Page 117 and 118: i rehab team or the BHF nurse, and/
- Page 119 and 120: i i i Referral to ICU should follow
- Page 121 and 122: ATRIAL FLUTTER Characterised by rap
- Page 123 and 124: i Seek senior cardiology advice reg
- Page 125 and 126: Causes • Bradycardia • Electrol
- Page 127 and 128: i i In anterior infarction the deve
- Page 129 and 130: abnormalities develop i.e. second o
- Page 131 and 132: i VASCULAR EMERGENCIES ACUTE THORAC
- Page 133 and 134: i ACUTE STROKE Stroke is a Medical
- Page 135 and 136: STROKE DIFFERENTIAL DIAGNOSIS: COND
- Page 137 and 138: ACUTE STROKE INTEGRATED CARE PATHWA
- Page 139 and 140: ST JOHN’S HOSPITAL CARE PATHWAY A
- Page 141 and 142: Role of D-dimer D-Dimer is helpful
- Page 143 and 144: i Thrombolysis bolus alteplase (rtP
- Page 145 and 146: i MANAGEMENT OF THE ACUTELY ISCHAEM
- Page 147 and 148: i Chapter 4 RESPIRATORY EMERGENCIES
- Page 149 and 150: i i • Decreased respiratory and h
- Page 151 and 152: i i • Co-morbidity. • Multiloba
- Page 153 and 154: other factors. Consult local antibi
- Page 155 and 156: Antibiotics • Amoxicillin (amoxyc
- Page 157 and 158: MANAGEMENT OF SPONTANEOUS PNEUMOTHO
- Page 159 and 160: • Look at the CXR and mark intuba
- Page 161 and 162:
pack. Advance slowly along the infi
- Page 163 and 164:
Figure 1a - preparing to insert a c
- Page 165 and 166:
i i MANAGEMENT OF CHEST DRAINS •
- Page 167 and 168:
Features of a major bleed? • Tach
- Page 169 and 170:
i i Contact GI Registrar. ROCKALL S
- Page 171 and 172:
i i • Blood, urine and ascitic fl
- Page 173 and 174:
• For alcoholic liver disease: th
- Page 175 and 176:
Known IBD • Exclude infection. Mi
- Page 177 and 178:
• Are any drugs implicated e.g. o
- Page 179 and 180:
ACUTE PANCREATITIS Determine severi
- Page 181 and 182:
then it would be more appropriate t
- Page 183 and 184:
RIE/WGH ACUTE SURGICAL ADMISSION IN
- Page 185 and 186:
i i VASCULAR: renal artery disease
- Page 187 and 188:
• Examine the urine: proteinuria
- Page 189 and 190:
i 1. IMMEDIATE ACTION: STABILISATIO
- Page 191 and 192:
METABOLIC ACIDOSIS CAUSES OF METABO
- Page 193 and 194:
i MANAGEMENT OF DIABETIC KETOACIDOS
- Page 195 and 196:
i Electrolyte replacement • Despi
- Page 197 and 198:
• Screen for myocardial infarctio
- Page 199 and 200:
• Monitor respiratory rate, ECG,
- Page 201 and 202:
Consider Precipitating Factors: •
- Page 203 and 204:
likely to be either GKI or sliding
- Page 205 and 206:
• If capillary blood glucose is g
- Page 207 and 208:
COMMON SYMPTOMS OF HYPOGLYCAEMIA Au
- Page 209 and 210:
Always discuss with the metabolic r
- Page 211 and 212:
• Abdominal pain • Depression
- Page 213 and 214:
• Hypoparathyroidism, surgical.
- Page 215 and 216:
i TREATMENT Oral • Sando K 2-3 ta
- Page 217 and 218:
• Measurement of plasma renin act
- Page 219 and 220:
Flow Chart for the assessment and m
- Page 221 and 222:
Chapter 7 NEUROLOGICAL EMERGENCIES
- Page 223 and 224:
AETIOLOGY OF COMA Primary neurologi
- Page 225 and 226:
EPILEPTIC SEIZURES Epilepsy is a sy
- Page 227 and 228:
i DRUGS Initial treatment is with D
- Page 229 and 230:
INDICATIONS FOR INTUBATION AND VENT
- Page 231 and 232:
LIKELY ORGANISMS • Depend on age,
- Page 233 and 234:
TENTORIAL HERNIATION AND CONING •
- Page 235 and 236:
• CT scan if focal neurology, rai
- Page 237 and 238:
• Assessment of cognition can be
- Page 239 and 240:
ACUTE AGITATED CONFUSION IN AN OLDE
- Page 241 and 242:
• Drugs: - polypharmacy (>4 drugs
- Page 243 and 244:
i Chapter 9 EMEGENCIES IN HAEMATOLO
- Page 245 and 246:
on waking, and may be aggravated by
- Page 247 and 248:
EMERGENCIES IN PALLIATIVE CARE Emer
- Page 249 and 250:
SEIZURES IN PALLIATIVE CARE Seizure
- Page 251 and 252:
NALOXONE IN PALLIATIVE CARE Naloxon
- Page 253 and 254:
CARE OF THE DYING PATIENT If you th
- Page 255 and 256:
THE ROLE OF JUNIOR MEDICAL STAFF IN
- Page 257 and 258:
• Ensure adequate ventilation. Tr
- Page 259 and 260:
• Paracetamol and salicylate conc
- Page 261 and 262:
MANAGEMENT OF COMMON POISONINGS Par
- Page 263 and 264:
i i treatment schedule should be us
- Page 265 and 266:
i Toxicity Serious toxicity from pu
- Page 267 and 268:
conscious level. • Correct electr
- Page 269 and 270:
• Correct metabolic acidosis with
- Page 271 and 272:
i SEPSIS • Any age, any joint, ma
- Page 273 and 274:
Reactive Arthritis • Bed rest plu
- Page 275 and 276:
N.B. Remember spontaneous bacterial
- Page 277 and 278:
i ALCOHOL WITHDRAWAL MANAGEMENT Ens
- Page 279 and 280:
ACUTE DISTURBANCE Guide for medical
- Page 281 and 282:
detention certificate must state th
- Page 283 and 284:
a person there. Under an EDC, treat
- Page 285 and 286:
Appendix 1 SHARING DIFFICULT INFORM
- Page 287 and 288:
1. Write down or review what you ar
- Page 289 and 290:
CHECKLIST OF REQUIREMENTS This chec
- Page 291 and 292:
i • Reactions vary: distress, ang
- Page 293 and 294:
• Damaged syringes and siphonage:
- Page 295 and 296:
Start-up time (Syringe pumps) What
- Page 297 and 298:
• HR increases by 17% and stroke
- Page 299 and 300:
PAEDIATRIC FBAO TREATMENT Assess se
- Page 301 and 302:
CONSENT TO MEDICAL TREATMENT FOR CH
- Page 303 and 304:
CONTRACEPTION AND ABORTION It would
- Page 305 and 306:
c) Drugs and catheterisation pack -
- Page 307 and 308:
INSTRUCTIONS FOR ANAESTHETIST + ODP
- Page 309 and 310:
DRUGS - CIRCULATING NURSE 1. MAKE S
- Page 311 and 312:
HELP - NURSE / RESIDENT The followi
- Page 313 and 314:
RECOVERY & FURTHER TREATMENT With r
- Page 315 and 316:
MAJOR HAEMORRHAGE PROTOCOL 314 adul
- Page 317:
Useful links The Anaphylaxis campai