Adult Medical Emergency Handbook - Scottish Intensive Care Society
Adult Medical Emergency Handbook - Scottish Intensive Care Society
Adult Medical Emergency Handbook - Scottish Intensive Care Society
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
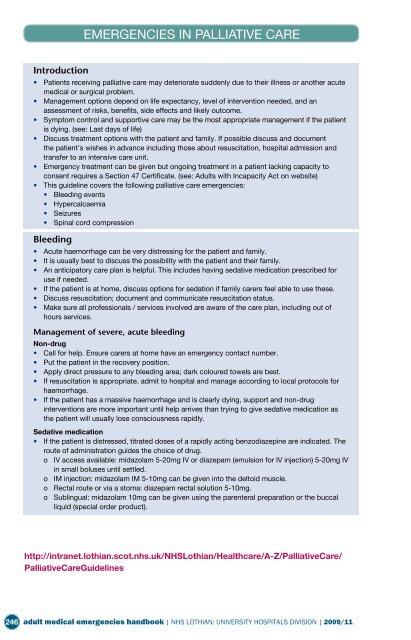
EMERGENCIES IN PALLIATIVE CARE<br />
Emergencies in Palliative <strong>Care</strong><br />
Introduction<br />
• Patients receiving palliative care may deteriorate suddenly due to their illness or another acute<br />
medical or surgical problem.<br />
• Management options depend on life expectancy, level of intervention needed, and an<br />
assessment of risks, benefits, side effects and likely outcome.<br />
• Symptom control and supportive care may be the most appropriate management if the patient<br />
is dying. (see: Last days of life)<br />
• Discuss treatment options with the patient and family. If possible discuss and document<br />
the patient’s wishes in advance including those about resuscitation, hospital admission and<br />
transfer to an intensive care unit.<br />
• <strong>Emergency</strong> treatment can be given but ongoing treatment in a patient lacking capacity to<br />
consent requires a Section 47 Certificate. (see: <strong>Adult</strong>s with Incapacity Act on website)<br />
• This guideline covers the following palliative care emergencies:<br />
• Bleeding events<br />
• Hypercalcaemia<br />
• Seizures<br />
• Spinal cord compression<br />
Bleeding<br />
• Acute haemorrhage can be very distressing for the patient and family.<br />
• It is usually best to discuss the possibility with the patient and their family.<br />
• An anticipatory care plan is helpful. This includes having sedative medication prescribed for<br />
use if needed.<br />
• If the patient is at home, discuss options for sedation if family carers feel able to use these.<br />
• Discuss resuscitation; document and communicate resuscitation status.<br />
• Make sure all professionals / services involved are aware of the care plan, including out of<br />
hours services.<br />
Management of severe, acute bleeding<br />
Non-drug<br />
• Call for help. Ensure carers at home have an emergency contact number.<br />
• Put the patient in the recovery position.<br />
• Apply direct pressure to any bleeding area; dark coloured towels are best.<br />
• If resuscitation is appropriate, admit to hospital and manage according to local protocols for<br />
haemorrhage.<br />
• If the patient has a massive haemorrhage and is clearly dying, support and non-drug<br />
interventions are more important until help arrives than trying to give sedative medication as<br />
the patient will usually lose consciousness rapidly.<br />
Sedative medication<br />
• If the patient is distressed, titrated doses of a rapidly acting benzodiazepine are indicated. The<br />
route of administration guides the choice of drug.<br />
o IV access available: midazolam 5-20mg IV or diazepam (emulsion for IV injection) 5-20mg IV<br />
in small boluses until settled.<br />
o IM injection: midazolam IM 5-10mg can be given into the deltoid muscle.<br />
o Rectal route or via a stoma: diazepam rectal solution 5-10mg.<br />
o Sublingual: midazolam 10mg can be given using the parenteral preparation or the buccal<br />
liquid (special order product).<br />
http://intranet.lothian.scot.nhs.uk/NHSLothian/Healthcare/A-Z/Palliative<strong>Care</strong>/<br />
Palliative<strong>Care</strong>Guidelines<br />
246 adult medical emergencies handbook | NHS LOTHIAN: UNIVERSITY HOSPITALS DIVISION | 2009/11