Clinical Pharmacology and Therapeutics
A Textbook of Clinical Pharmacology and ... - clinicalevidence
A Textbook of Clinical Pharmacology and ... - clinicalevidence
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
112 SCHIZOPHRENIA AND BEHAVIOURAL EMERGENCIES<br />
DRUGS USED IN TREATMENT<br />
CONVENTIONAL ANTIPSYCHOTIC DRUGS<br />
The principal action of the conventional antipsychotic drugs<br />
(see Table 19.1), such as chlorpromazine (a phenothiazine) <strong>and</strong><br />
haloperidol (a butyrophenone), is an antagonism of D 2 receptors<br />
in the forebrain. The effect on D 1 receptors is variable.<br />
Blockade of the D 2 receptors induces extrapyramidal effects.<br />
Repeated adminstration causes an increase in D 2 -receptor sensitivity<br />
due to an increase in abundance of these receptors. This<br />
appears to underlie the tardive dyskinesias that are caused by<br />
prolonged use of the conventional antipsychotic drugs.<br />
The choice of drug is largely determined by the dem<strong>and</strong>s of<br />
the clinical situation, in particular the degree of sedation<br />
needed <strong>and</strong> the patient’s susceptibility to extrapyramidal toxicity<br />
<strong>and</strong> hypotension.<br />
Uses<br />
These include the following:<br />
1. schizophrenia – antipsychotic drugs are more effective<br />
against first-rank (positive) symptoms (hallucinations,<br />
thought disorder, delusions, feelings of external control)<br />
than against negative symptoms (apathy <strong>and</strong><br />
withdrawal);<br />
2. other excited psychotic states, including mania <strong>and</strong><br />
delirium;<br />
3. anti-emetic <strong>and</strong> anti-hiccough;<br />
4. premedication <strong>and</strong> in neuroleptanalgesia;<br />
5. terminal illness, including potentiating desired actions of<br />
opioids while reducing nausea <strong>and</strong> vomiting;<br />
6. severe agitation <strong>and</strong> panic;<br />
7. aggressive <strong>and</strong> violent behaviour;<br />
8. movement <strong>and</strong> mental disorders in Huntington’s disease.<br />
Adverse effects<br />
1. The most common adverse effects are dose-dependent<br />
extensions of pharmacological actions:<br />
• extrapyramidal symptoms (related to tight binding to,<br />
<strong>and</strong> receptor occupancy of, D 2 receptors) – parkinsonism<br />
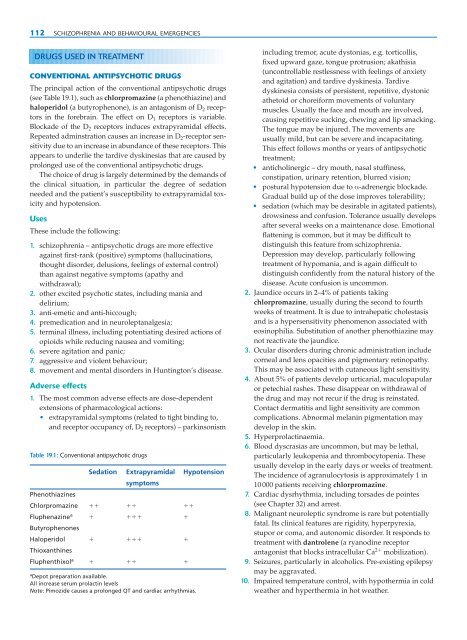
Table 19.1: Conventional antipsychotic drugs<br />
Sedation Extrapyramidal Hypotension<br />
symptoms<br />
Phenothiazines<br />
Chlorpromazine <br />
Fluphenazine a <br />
Butyrophenones<br />
Haloperidol <br />
Thioxanthines<br />
Fluphenthixol a <br />
a Depot preparation available.<br />
All increase serum prolactin levels<br />
Note: Pimozide causes a prolonged QT <strong>and</strong> cardiac arrhythmias.<br />
including tremor, acute dystonias, e.g. torticollis,<br />
fixed upward gaze, tongue protrusion; akathisia<br />
(uncontrollable restlessness with feelings of anxiety<br />
<strong>and</strong> agitation) <strong>and</strong> tardive dyskinesia. Tardive<br />
dyskinesia consists of persistent, repetitive, dystonic<br />
athetoid or choreiform movements of voluntary<br />
muscles. Usually the face <strong>and</strong> mouth are involved,<br />
causing repetitive sucking, chewing <strong>and</strong> lip smacking.<br />
The tongue may be injured. The movements are<br />
usually mild, but can be severe <strong>and</strong> incapacitating.<br />
This effect follows months or years of antipsychotic<br />
treatment;<br />
• anticholinergic – dry mouth, nasal stuffiness,<br />
constipation, urinary retention, blurred vision;<br />
• postural hypotension due to α-adrenergic blockade.<br />
Gradual build up of the dose improves tolerability;<br />
• sedation (which may be desirable in agitated patients),<br />
drowsiness <strong>and</strong> confusion. Tolerance usually develops<br />
after several weeks on a maintenance dose. Emotional<br />
flattening is common, but it may be difficult to<br />
distinguish this feature from schizophrenia.<br />
Depression may develop, particularly following<br />
treatment of hypomania, <strong>and</strong> is again difficult to<br />
distinguish confidently from the natural history of the<br />
disease. Acute confusion is uncommon.<br />
2. Jaundice occurs in 2–4% of patients taking<br />
chlorpromazine, usually during the second to fourth<br />
weeks of treatment. It is due to intrahepatic cholestasis<br />
<strong>and</strong> is a hypersensitivity phenomenon associated with<br />
eosinophilia. Substitution of another phenothiazine may<br />
not reactivate the jaundice.<br />
3. Ocular disorders during chronic administration include<br />
corneal <strong>and</strong> lens opacities <strong>and</strong> pigmentary retinopathy.<br />
This may be associated with cutaneous light sensitivity.<br />
4. About 5% of patients develop urticarial, maculopapular<br />
or petechial rashes. These disappear on withdrawal of<br />
the drug <strong>and</strong> may not recur if the drug is reinstated.<br />
Contact dermatitis <strong>and</strong> light sensitivity are common<br />
complications. Abnormal melanin pigmentation may<br />
develop in the skin.<br />
5. Hyperprolactinaemia.<br />
6. Blood dyscrasias are uncommon, but may be lethal,<br />
particularly leukopenia <strong>and</strong> thrombocytopenia. These<br />
usually develop in the early days or weeks of treatment.<br />
The incidence of agranulocytosis is approximately 1 in<br />
10 000 patients receiving chlorpromazine.<br />
7. Cardiac dysrhythmia, including torsades de pointes<br />
(see Chapter 32) <strong>and</strong> arrest.<br />
8. Malignant neuroleptic syndrome is rare but potentially<br />
fatal. Its clinical features are rigidity, hyperpyrexia,<br />
stupor or coma, <strong>and</strong> autonomic disorder. It responds to<br />
treatment with dantrolene (a ryanodine receptor<br />
antagonist that blocks intracellular Ca 2 mobilization).<br />
9. Seizures, particularly in alcoholics. Pre-existing epilepsy<br />
may be aggravated.<br />
10. Impaired temperature control, with hypothermia in cold<br />
weather <strong>and</strong> hyperthermia in hot weather.