Clinical Pharmacology and Therapeutics
A Textbook of Clinical Pharmacology and ... - clinicalevidence
A Textbook of Clinical Pharmacology and ... - clinicalevidence
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
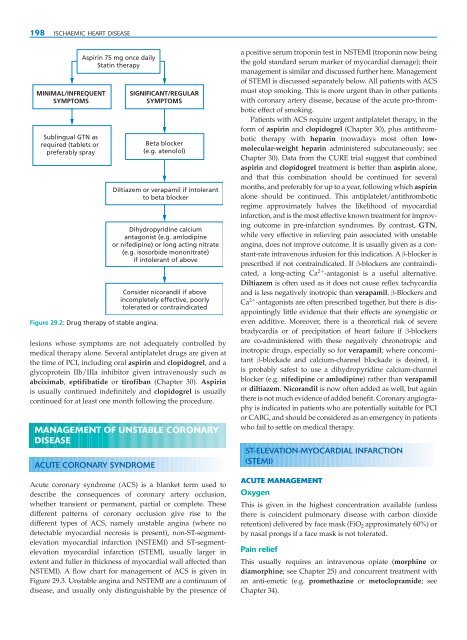
198 ISCHAEMIC HEART DISEASE<br />
MINIMAL/INFREQUENT<br />
SYMPTOMS<br />
Sublingual GTN as<br />
required (tablets or<br />
preferably spray<br />
Aspirin 75 mg once daily<br />
Statin therapy<br />
Figure 29.2: Drug therapy of stable angina.<br />
lesions whose symptoms are not adequately controlled by<br />
medical therapy alone. Several antiplatelet drugs are given at<br />
the time of PCI, including oral aspirin <strong>and</strong> clopidogrel, <strong>and</strong> a<br />
glycoprotein IIb/IIIa inhibitor given intravenously such as<br />
abciximab, eptifibatide or tirofiban (Chapter 30). Aspirin<br />
is usually continued indefinitely <strong>and</strong> clopidogrel is usually<br />
continued for at least one month following the procedure.<br />
MANAGEMENT OF UNSTABLE CORONARY<br />
DISEASE<br />
ACUTE CORONARY SYNDROME<br />
SIGNIFICANT/REGULAR<br />
SYMPTOMS<br />
Beta blocker<br />
(e.g. atenolol)<br />
Diltiazem or verapamil if intolerant<br />
to beta blocker<br />
Dihydropyridine calcium<br />
antagonist (e.g. amlodipine<br />
or nifedipine) or long acting nitrate<br />
(e.g. isosorbide mononitrate)<br />
if intolerant of above<br />
Consider nicor<strong>and</strong>il if above<br />
incompletely effective, poorly<br />
tolerated or contraindicated<br />
Acute coronary syndrome (ACS) is a blanket term used to<br />
describe the consequences of coronary artery occlusion,<br />
whether transient or permanent, partial or complete. These<br />
different patterns of coronary occlusion give rise to the<br />
different types of ACS, namely unstable angina (where no<br />
detectable myocardial necrosis is present), non-ST-segmentelevation<br />
myocardial infarction (NSTEMI) <strong>and</strong> ST-segmentelevation<br />
myocardial infarction (STEMI, usually larger in<br />
extent <strong>and</strong> fuller in thickness of myocardial wall affected than<br />
NSTEMI). A flow chart for management of ACS is given in<br />
Figure 29.3. Unstable angina <strong>and</strong> NSTEMI are a continuum of<br />
disease, <strong>and</strong> usually only distinguishable by the presence of<br />
a positive serum troponin test in NSTEMI (troponin now being<br />
the gold st<strong>and</strong>ard serum marker of myocardial damage); their<br />
management is similar <strong>and</strong> discussed further here. Management<br />
of STEMI is discussed separately below. All patients with ACS<br />
must stop smoking. This is more urgent than in other patients<br />
with coronary artery disease, because of the acute pro-thrombotic<br />
effect of smoking.<br />
Patients with ACS require urgent antiplatelet therapy, in the<br />
form of aspirin <strong>and</strong> clopidogrel (Chapter 30), plus antithrombotic<br />
therapy with heparin (nowadays most often lowmolecular-weight<br />
heparin administered subcutaneously; see<br />
Chapter 30). Data from the CURE trial suggest that combined<br />
aspirin <strong>and</strong> clopidogrel treatment is better than aspirin alone,<br />
<strong>and</strong> that this combination should be continued for several<br />
months, <strong>and</strong> preferably for up to a year, following which aspirin<br />
alone should be continued. This antiplatelet/antithrombotic<br />
regime approximately halves the likelihood of myocardial<br />
infarction, <strong>and</strong> is the most effective known treatment for improving<br />
outcome in pre-infarction syndromes. By contrast, GTN,<br />
while very effective in relieving pain associated with unstable<br />
angina, does not improve outcome. It is usually given as a constant-rate<br />
intravenous infusion for this indication. A β-blocker is<br />
prescribed if not contraindicated. If β-blockers are contraindicated,<br />
a long-acting Ca 2 -antagonist is a useful alternative.<br />
Diltiazem is often used as it does not cause reflex tachycardia<br />
<strong>and</strong> is less negatively inotropic than verapamil. β-Blockers <strong>and</strong><br />
Ca 2 -antagonists are often prescribed together, but there is disappointingly<br />
little evidence that their effects are synergistic or<br />
even additive. Moreover, there is a theoretical risk of severe<br />
bradycardia or of precipitation of heart failure if β-blockers<br />
are co-administered with these negatively chronotropic <strong>and</strong><br />
inotropic drugs, especially so for verapamil; where concomitant<br />
β-blockade <strong>and</strong> calcium-channel blockade is desired, it<br />
is probably safest to use a dihydropyridine calcium-channel<br />
blocker (e.g. nifedipine or amlodipine) rather than verapamil<br />
or diltiazem. Nicor<strong>and</strong>il is now often added as well, but again<br />
there is not much evidence of added benefit. Coronary angiography<br />
is indicated in patients who are potentially suitable for PCI<br />
or CABG, <strong>and</strong> should be considered as an emergency in patients<br />
who fail to settle on medical therapy.<br />
ST-ELEVATION-MYOCARDIAL INFARCTION<br />
(STEMI)<br />
ACUTE MANAGEMENT<br />
Oxygen<br />
This is given in the highest concentration available (unless<br />
there is coincident pulmonary disease with carbon dioxide<br />
retention) delivered by face mask (FiO 2 approximately 60%) or<br />
by nasal prongs if a face mask is not tolerated.<br />
Pain relief<br />
This usually requires an intravenous opiate (morphine or<br />
diamorphine; see Chapter 25) <strong>and</strong> concurrent treatment with<br />
an anti-emetic (e.g. promethazine or metoclopramide; see<br />
Chapter 34).