Clinical Pharmacology and Therapeutics
A Textbook of Clinical Pharmacology and ... - clinicalevidence
A Textbook of Clinical Pharmacology and ... - clinicalevidence
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
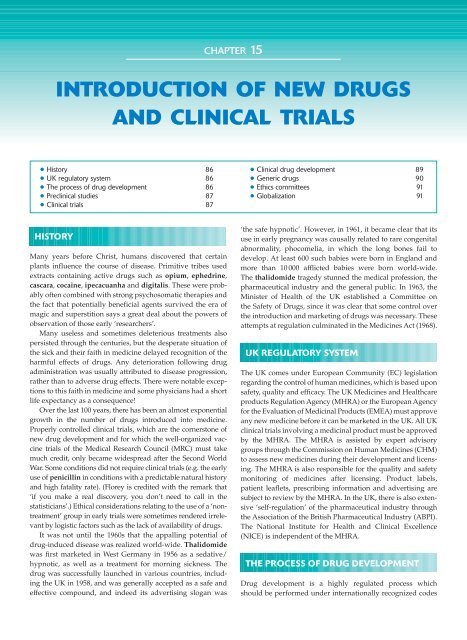
CHAPTER 15<br />
INTRODUCTION OF NEW DRUGS<br />
AND CLINICAL TRIALS<br />
● History 86<br />
● UK regulatory system 86<br />
● The process of drug development 86<br />
● Preclinical studies 87<br />
● <strong>Clinical</strong> trials 87<br />
● <strong>Clinical</strong> drug development 89<br />
● Generic drugs 90<br />
● Ethics committees 91<br />
● Globalization 91<br />
HISTORY<br />
Many years before Christ, humans discovered that certain<br />
plants influence the course of disease. Primitive tribes used<br />
extracts containing active drugs such as opium, ephedrine,<br />
cascara, cocaine, ipecacuanha <strong>and</strong> digitalis. These were probably<br />
often combined with strong psychosomatic therapies <strong>and</strong><br />
the fact that potentially beneficial agents survived the era of<br />
magic <strong>and</strong> superstition says a great deal about the powers of<br />
observation of those early ‘researchers’.<br />
Many useless <strong>and</strong> sometimes deleterious treatments also<br />
persisted through the centuries, but the desperate situation of<br />
the sick <strong>and</strong> their faith in medicine delayed recognition of the<br />
harmful effects of drugs. Any deterioration following drug<br />
administration was usually attributed to disease progression,<br />
rather than to adverse drug effects. There were notable exceptions<br />
to this faith in medicine <strong>and</strong> some physicians had a short<br />
life expectancy as a consequence!<br />
Over the last 100 years, there has been an almost exponential<br />
growth in the number of drugs introduced into medicine.<br />
Properly controlled clinical trials, which are the cornerstone of<br />
new drug development <strong>and</strong> for which the well-organized vaccine<br />
trials of the Medical Research Council (MRC) must take<br />
much credit, only became widespread after the Second World<br />
War. Some conditions did not require clinical trials (e.g. the early<br />
use of penicillin in conditions with a predictable natural history<br />
<strong>and</strong> high fatality rate). (Florey is credited with the remark that<br />
‘if you make a real discovery, you don’t need to call in the<br />
statisticians’.) Ethical considerations relating to the use of a ‘nontreatment’<br />
group in early trials were sometimes rendered irrelevant<br />
by logistic factors such as the lack of availability of drugs.<br />
It was not until the 1960s that the appalling potential of<br />
drug-induced disease was realized world-wide. Thalidomide<br />
was first marketed in West Germany in 1956 as a sedative/<br />
hypnotic, as well as a treatment for morning sickness. The<br />
drug was successfully launched in various countries, including<br />
the UK in 1958, <strong>and</strong> was generally accepted as a safe <strong>and</strong><br />
effective compound, <strong>and</strong> indeed its advertising slogan was<br />
‘the safe hypnotic’. However, in 1961, it became clear that its<br />
use in early pregnancy was causally related to rare congenital<br />
abnormality, phocomelia, in which the long bones fail to<br />
develop. At least 600 such babies were born in Engl<strong>and</strong> <strong>and</strong><br />
more than 10 000 afflicted babies were born world-wide.<br />
The thalidomide tragedy stunned the medical profession, the<br />
pharmaceutical industry <strong>and</strong> the general public. In 1963, the<br />
Minister of Health of the UK established a Committee on<br />
the Safety of Drugs, since it was clear that some control over<br />
the introduction <strong>and</strong> marketing of drugs was necessary. These<br />
attempts at regulation culminated in the Medicines Act (1968).<br />
UK REGULATORY SYSTEM<br />
The UK comes under European Community (EC) legislation<br />
regarding the control of human medicines, which is based upon<br />
safety, quality <strong>and</strong> efficacy. The UK Medicines <strong>and</strong> Healthcare<br />
products Regulation Agency (MHRA) or the European Agency<br />
for the Evaluation of Medicinal Products (EMEA) must approve<br />
any new medicine before it can be marketed in the UK. All UK<br />
clinical trials involving a medicinal product must be approved<br />
by the MHRA. The MHRA is assisted by expert advisory<br />
groups through the Commission on Human Medicines (CHM)<br />
to assess new medicines during their development <strong>and</strong> licensing.<br />
The MHRA is also responsible for the quality <strong>and</strong> safety<br />
monitoring of medicines after licensing. Product labels,<br />
patient leaflets, prescribing information <strong>and</strong> advertising are<br />
subject to review by the MHRA. In the UK, there is also extensive<br />
‘self-regulation’ of the pharmaceutical industry through<br />
the Association of the British Pharmaceutical Industry (ABPI).<br />
The National Institute for Health <strong>and</strong> <strong>Clinical</strong> Excellence<br />
(NICE) is independent of the MHRA.<br />
THE PROCESS OF DRUG DEVELOPMENT<br />
Drug development is a highly regulated process which<br />
should be performed under internationally recognized codes