Clinical Pharmacology and Therapeutics
A Textbook of Clinical Pharmacology and ... - clinicalevidence
A Textbook of Clinical Pharmacology and ... - clinicalevidence
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
338 MYCOBACTERIAL INFECTIONS<br />
Mechanism of action<br />
Like other aminoglycosides, it is actively transported across<br />
the bacterial cell wall, <strong>and</strong> its antibacterial activity is due to<br />
specific binding to the P12 protein on the 30S subunit of the<br />
bacterial ribosome, inhibiting protein synthesis.<br />
Adverse effects<br />
These are the same as for other aminoglycosides (see Chapter 43).<br />
The major side effects are eighth nerve toxicity (vestibulotoxicity<br />
more than deafness), nephrotoxicity <strong>and</strong>, less commonly, allergic<br />
reactions.<br />
Contraindications<br />
Streptomycin is contraindicated in patients with eighth nerve<br />
dysfunction, in those who are pregnant <strong>and</strong> in those with myasthenia<br />
gravis, as it has weak neuromuscular blocking activity.<br />
Pharmacokinetics<br />
Oral absorption is minimal <strong>and</strong> it is given intramuscularly.<br />
Streptomycin is mainly excreted via the kidney <strong>and</strong> renal<br />
impairment requires dose adjustment. The t 1/2 of streptomycin<br />
is in the range of two to nine hours. It crosses the blood–brain<br />
barrier when the meninges are inflamed.<br />
PREPARATIONS CONTAINING COMBINED<br />
ANTI-TUBERCULOUS DRUGS<br />
Several combination preparations of the first-line drugs are<br />
available. They are helpful when patients are established<br />
on therapy, <strong>and</strong> the reduced number of tablets should aid compliance<br />
<strong>and</strong> avoid monotherapy. Combined preparations available<br />
include Mynah (ethambutol <strong>and</strong> INH, in varying<br />
dosages), Rifinah <strong>and</strong> Rimactazid (containing rifampicin<br />
<strong>and</strong> INH) <strong>and</strong> Rifater (containing INH, rifampicin <strong>and</strong><br />
pyrazinamide).<br />
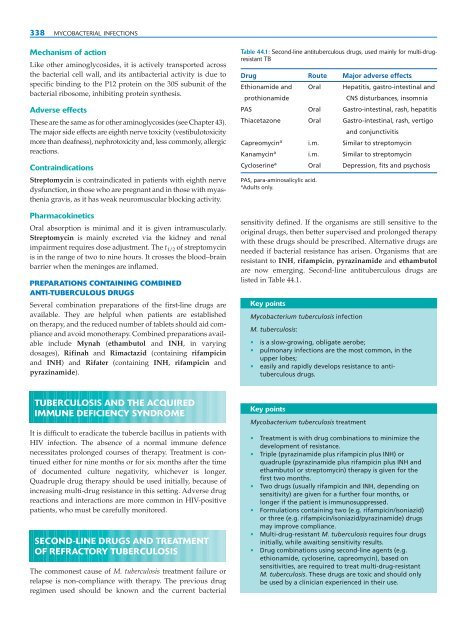
Table 44.1: Second-line antituberculous drugs, used mainly for multi-drugresistant<br />
TB<br />
Drug Route Major adverse effects<br />
Ethionamide <strong>and</strong> Oral Hepatitis, gastro-intestinal <strong>and</strong><br />
prothionamide<br />
CNS disturbances, insomnia<br />
PAS Oral Gastro-intestinal, rash, hepatitis<br />
Thiacetazone Oral Gastro-intestinal, rash, vertigo<br />
<strong>and</strong> conjunctivitis<br />
Capreomycin a i.m. Similar to streptomycin<br />
Kanamycin a i.m. Similar to streptomycin<br />
Cycloserine a Oral Depression, fits <strong>and</strong> psychosis<br />
PAS, para-aminosalicylic acid.<br />
a Adults only.<br />
sensitivity defined. If the organisms are still sensitive to the<br />
original drugs, then better supervised <strong>and</strong> prolonged therapy<br />
with these drugs should be prescribed. Alternative drugs are<br />
needed if bacterial resistance has arisen. Organisms that are<br />
resistant to INH, rifampicin, pyrazinamide <strong>and</strong> ethambutol<br />
are now emerging. Second-line antituberculous drugs are<br />
listed in Table 44.1.<br />
Key points<br />
Mycobacterium tuberculosis infection<br />
M. tuberculosis:<br />
• is a slow-growing, obligate aerobe;<br />
• pulmonary infections are the most common, in the<br />
upper lobes;<br />
• easily <strong>and</strong> rapidly develops resistance to antituberculous<br />
drugs.<br />
TUBERCULOSIS AND THE ACQUIRED<br />
IMMUNE DEFICIENCY SYNDROME<br />
It is difficult to eradicate the tubercle bacillus in patients with<br />
HIV infection. The absence of a normal immune defence<br />
necessitates prolonged courses of therapy. Treatment is continued<br />
either for nine months or for six months after the time<br />
of documented culture negativity, whichever is longer.<br />
Quadruple drug therapy should be used initially, because of<br />
increasing multi-drug resistance in this setting. Adverse drug<br />
reactions <strong>and</strong> interactions are more common in HIV-positive<br />
patients, who must be carefully monitored.<br />
SECOND-LINE DRUGS AND TREATMENT<br />
OF REFRACTORY TUBERCULOSIS<br />
The commonest cause of M. tuberculosis treatment failure or<br />
relapse is non-compliance with therapy. The previous drug<br />
regimen used should be known <strong>and</strong> the current bacterial<br />
Key points<br />
Mycobacterium tuberculosis treatment<br />
• Treatment is with drug combinations to minimize the<br />
development of resistance.<br />
• Triple (pyrazinamide plus rifampicin plus INH) or<br />
quadruple (pyrazinamide plus rifampicin plus INH <strong>and</strong><br />
ethambutol or streptomycin) therapy is given for the<br />
first two months.<br />
• Two drugs (usually rifampicin <strong>and</strong> INH, depending on<br />
sensitivity) are given for a further four months, or<br />
longer if the patient is immunosuppressed.<br />
• Formulations containing two (e.g. rifampicin/isoniazid)<br />
or three (e.g. rifampicin/isoniazid/pyrazinamide) drugs<br />
may improve compliance.<br />
• Multi-drug-resistant M. tuberculosis requires four drugs<br />
initially, while awaiting sensitivity results.<br />
• Drug combinations using second-line agents (e.g.<br />
ethionamide, cycloserine, capreomycin), based on<br />
sensitivities, are required to treat multi-drug-resistant<br />
M. tuberculosis. These drugs are toxic <strong>and</strong> should only<br />
be used by a clinician experienced in their use.