Clinical Pharmacology and Therapeutics
A Textbook of Clinical Pharmacology and ... - clinicalevidence
A Textbook of Clinical Pharmacology and ... - clinicalevidence
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
CENTRAL DEPRESSANTS 441<br />
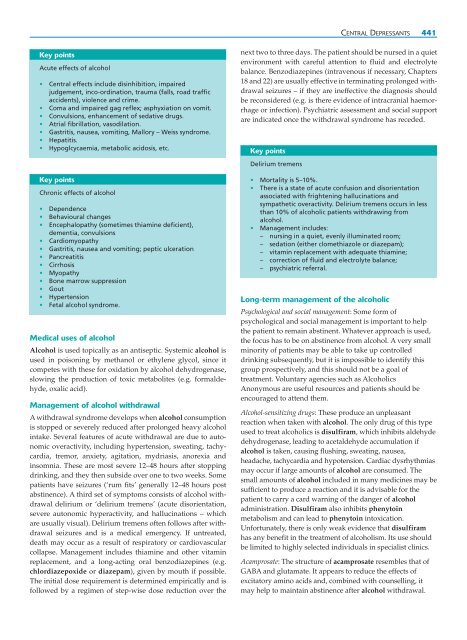
Key points<br />
Acute effects of alcohol<br />
• Central effects include disinhibition, impaired<br />
judgement, inco-ordination, trauma (falls, road traffic<br />
accidents), violence <strong>and</strong> crime.<br />
• Coma <strong>and</strong> impaired gag reflex; asphyxiation on vomit.<br />
• Convulsions, enhancement of sedative drugs.<br />
• Atrial fibrillation, vasodilation.<br />
• Gastritis, nausea, vomiting, Mallory – Weiss syndrome.<br />
• Hepatitis.<br />
• Hypoglcycaemia, metabolic acidosis, etc.<br />
Key points<br />
Chronic effects of alcohol<br />
• Dependence<br />
• Behavioural changes<br />
• Encephalopathy (sometimes thiamine deficient),<br />
dementia, convulsions<br />
• Cardiomyopathy<br />
• Gastritis, nausea <strong>and</strong> vomiting; peptic ulceration<br />
• Pancreatitis<br />
• Cirrhosis<br />
• Myopathy<br />
• Bone marrow suppression<br />
• Gout<br />
• Hypertension<br />
• Fetal alcohol syndrome.<br />
Medical uses of alcohol<br />
Alcohol is used topically as an antiseptic. Systemic alcohol is<br />
used in poisoning by methanol or ethylene glycol, since it<br />
competes with these for oxidation by alcohol dehydrogenase,<br />
slowing the production of toxic metabolites (e.g. formaldehyde,<br />
oxalic acid).<br />
Management of alcohol withdrawal<br />
A withdrawal syndrome develops when alcohol consumption<br />
is stopped or severely reduced after prolonged heavy alcohol<br />
intake. Several features of acute withdrawal are due to autonomic<br />
overactivity, including hypertension, sweating, tachycardia,<br />
tremor, anxiety, agitation, mydriasis, anorexia <strong>and</strong><br />
insomnia. These are most severe 12–48 hours after stopping<br />
drinking, <strong>and</strong> they then subside over one to two weeks. Some<br />
patients have seizures (‘rum fits’ generally 12–48 hours post<br />
abstinence). A third set of symptoms consists of alcohol withdrawal<br />
delirium or ‘delirium tremens’ (acute disorientation,<br />
severe autonomic hyperactivity, <strong>and</strong> hallucinations – which<br />
are usually visual). Delirium tremens often follows after withdrawal<br />
seizures <strong>and</strong> is a medical emergency. If untreated,<br />
death may occur as a result of respiratory or cardiovascular<br />
collapse. Management includes thiamine <strong>and</strong> other vitamin<br />
replacement, <strong>and</strong> a long-acting oral benzodiazepines (e.g.<br />
chlordiazepoxide or diazepam), given by mouth if possible.<br />
The initial dose requirement is determined empirically <strong>and</strong> is<br />
followed by a regimen of step-wise dose reduction over the<br />
next two to three days. The patient should be nursed in a quiet<br />
environment with careful attention to fluid <strong>and</strong> electrolyte<br />
balance. Benzodiazepines (intravenous if necessary, Chapters<br />
18 <strong>and</strong> 22) are usually effective in terminating prolonged withdrawal<br />
seizures – if they are ineffective the diagnosis should<br />
be reconsidered (e.g. is there evidence of intracranial haemorrhage<br />
or infection). Psychiatric assessment <strong>and</strong> social support<br />
are indicated once the withdrawal syndrome has receded.<br />
Key points<br />
Delirium tremens<br />
• Mortality is 5–10%.<br />
• There is a state of acute confusion <strong>and</strong> disorientation<br />
associated with frightening hallucinations <strong>and</strong><br />
sympathetic overactivity. Delirium tremens occurs in less<br />
than 10% of alcoholic patients withdrawing from<br />
alcohol.<br />
• Management includes:<br />
– nursing in a quiet, evenly illuminated room;<br />
– sedation (either clomethiazole or diazepam);<br />
– vitamin replacement with adequate thiamine;<br />
– correction of fluid <strong>and</strong> electrolyte balance;<br />
– psychiatric referral.<br />
Long-term management of the alcoholic<br />
Psychological <strong>and</strong> social management: Some form of<br />
psychological <strong>and</strong> social management is important to help<br />
the patient to remain abstinent. Whatever approach is used,<br />
the focus has to be on abstinence from alcohol. A very small<br />
minority of patients may be able to take up controlled<br />
drinking subsequently, but it is impossible to identify this<br />
group prospectively, <strong>and</strong> this should not be a goal of<br />
treatment. Voluntary agencies such as Alcoholics<br />
Anonymous are useful resources <strong>and</strong> patients should be<br />
encouraged to attend them.<br />
Alcohol-sensitizing drugs: These produce an unpleasant<br />
reaction when taken with alcohol. The only drug of this type<br />
used to treat alcoholics is disulfiram, which inhibits aldehyde<br />
dehydrogenase, leading to acetaldehyde accumulation if<br />
alcohol is taken, causing flushing, sweating, nausea,<br />
headache, tachycardia <strong>and</strong> hypotension. Cardiac dysrhythmias<br />
may occur if large amounts of alcohol are consumed. The<br />
small amounts of alcohol included in many medicines may be<br />
sufficient to produce a reaction <strong>and</strong> it is advisable for the<br />
patient to carry a card warning of the danger of alcohol<br />
administration. Disulfiram also inhibits phenytoin<br />
metabolism <strong>and</strong> can lead to phenytoin intoxication.<br />
Unfortunately, there is only weak evidence that disulfiram<br />
has any benefit in the treatment of alcoholism. Its use should<br />
be limited to highly selected individuals in specialist clinics.<br />
Acamprosate: The structure of acamprosate resembles that of<br />
GABA <strong>and</strong> glutamate. It appears to reduce the effects of<br />
excitatory amino acids <strong>and</strong>, combined with counselling, it<br />
may help to maintain abstinence after alcohol withdrawal.