Clinical Pharmacology and Therapeutics
A Textbook of Clinical Pharmacology and ... - clinicalevidence
A Textbook of Clinical Pharmacology and ... - clinicalevidence
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
THYROID DISEASE 39<br />
DIGOXIN<br />
Myxoedematous patients are extremely sensitive to digoxin,<br />
whereas unusually high doses are required in thyrotoxicosis.<br />
In general, hyperthyroid patients have lower plasma digoxin<br />
concentrations <strong>and</strong> hypothyroid patients have higher plasma<br />
concentrations than euthyroid patients on the same dose.<br />
There is no significant difference in half-life between these<br />
groups, <strong>and</strong> a difference in V d has been postulated to explain<br />
the alteration of plasma concentration with thyroid activity.<br />
Changes in renal function, which occur with changes in thyroid<br />
status, complicate this interpretation. GFR is increased in<br />
thyrotoxicosis <strong>and</strong> decreased in myxoedema. These changes<br />
in renal function influence elimination, <strong>and</strong> the reduced plasma<br />
levels of digoxin correlate closely with the increased creatinine<br />
clearance in thyrotoxicosis. Other factors including enhanced<br />
biliary clearance, digoxin malabsorption due to intestinal<br />
hurry <strong>and</strong> increased hepatic metabolism, have all been postulated<br />
as factors contributing to the insensitivity of thyrotoxic<br />
patients to cardiac glycosides.<br />
ANTICOAGULANTS<br />
Oral anticoagulants produce an exaggerated prolongation of<br />
prothrombin time in hyperthyroid patients. This is due to<br />
increased metabolic breakdown of vitamin K-dependent clotting<br />
factors (Chapter 30), rather than to changes in drug pharmacokinetics.<br />
GLUCOCORTICOIDS<br />
Glucocorticoids are metabolized by hepatic mixed-function<br />
oxidases (CYP3A4) which are influenced by thyroid status.<br />
In hyperthyroidism, there is increased cortisol production<br />
<strong>and</strong> a reduced cortisol half-life, the converse being true in<br />
myxoedema.<br />
THYROXINE<br />
The normal half-life of thyroxine (six to seven days) is reduced<br />
to three to four days by hyperthyroidism <strong>and</strong> prolonged to<br />
nine to ten days by hypothyroidism. This is of considerable<br />
clinical importance when deciding on an appropriate interval<br />
at which to increase the dose of thyroxine in patients treated<br />
for myxoedema, especially if they have coincident ischaemic<br />
heart disease which would be exacerbated if an excessive<br />
steady-state thyroxine level were achieved.<br />
ANTITHYROID DRUGS<br />
The half-life of propylthiouracil <strong>and</strong> methimazole is prolonged<br />
in hypothyroidism <strong>and</strong> shortened in hyperthyroidism.<br />
These values return to normal on attainment of the euthyroid<br />
state, probably because of altered hepatic metabolism.<br />
OPIATES<br />
Patients with hypothyroidism are exceptionally sensitive to<br />
opioid analgesics, which cause profound respiratory depression<br />
in this setting. This is probably due to reduced metabolism<br />
<strong>and</strong> increased sensitivity.<br />
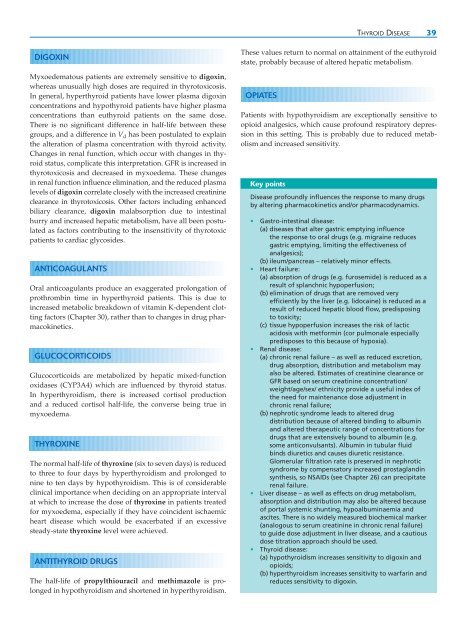
Key points<br />
Disease profoundly influences the response to many drugs<br />
by altering pharmacokinetics <strong>and</strong>/or pharmacodynamics.<br />
• Gastro-intestinal disease:<br />
(a) diseases that alter gastric emptying influence<br />
the response to oral drugs (e.g. migraine reduces<br />
gastric emptying, limiting the effectiveness of<br />
analgesics);<br />
(b) ileum/pancreas – relatively minor effects.<br />
• Heart failure:<br />
(a) absorption of drugs (e.g. furosemide) is reduced as a<br />
result of splanchnic hypoperfusion;<br />
(b) elimination of drugs that are removed very<br />
efficiently by the liver (e.g. lidocaine) is reduced as a<br />
result of reduced hepatic blood flow, predisposing<br />
to toxicity;<br />
(c) tissue hypoperfusion increases the risk of lactic<br />
acidosis with metformin (cor pulmonale especially<br />
predisposes to this because of hypoxia).<br />
• Renal disease:<br />
(a) chronic renal failure – as well as reduced excretion,<br />
drug absorption, distribution <strong>and</strong> metabolism may<br />
also be altered. Estimates of creatinine clearance or<br />
GFR based on serum creatinine concentration/<br />
weight/age/sex/ ethnicity provide a useful index of<br />
the need for maintenance dose adjustment in<br />
chronic renal failure;<br />
(b) nephrotic syndrome leads to altered drug<br />
distribution because of altered binding to albumin<br />
<strong>and</strong> altered therapeutic range of concentrations for<br />
drugs that are extensively bound to albumin (e.g.<br />
some anticonvulsants). Albumin in tubular fluid<br />
binds diuretics <strong>and</strong> causes diuretic resistance.<br />
Glomerular filtration rate is preserved in nephrotic<br />
syndrome by compensatory increased prostagl<strong>and</strong>in<br />
synthesis, so NSAIDs (see Chapter 26) can precipitate<br />
renal failure.<br />
• Liver disease – as well as effects on drug metabolism,<br />
absorption <strong>and</strong> distribution may also be altered because<br />
of portal systemic shunting, hypoalbuminaemia <strong>and</strong><br />
ascites. There is no widely measured biochemical marker<br />
(analogous to serum creatinine in chronic renal failure)<br />
to guide dose adjustment in liver disease, <strong>and</strong> a cautious<br />
dose titration approach should be used.<br />
• Thyroid disease:<br />
(a) hypothyroidism increases sensitivity to digoxin <strong>and</strong><br />
opioids;<br />
(b) hyperthyroidism increases sensitivity to warfarin <strong>and</strong><br />
reduces sensitivity to digoxin.