Clinical Pharmacology and Therapeutics
A Textbook of Clinical Pharmacology and ... - clinicalevidence
A Textbook of Clinical Pharmacology and ... - clinicalevidence
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
228 CARDIAC DYSRHYTHMIAS<br />
deficiency, since Mg 2 is predominantly an intracellular cation.<br />
However, serial plasma magnesium determinations may be<br />
useful in preventing excessive dosing with accumulation <strong>and</strong><br />
toxicity.<br />
Mechanism of action<br />
Mg 2 is a divalent cation <strong>and</strong> at least some of its beneficial<br />
effects are probably due to the consequent neutralization of<br />
fixed negative charges on the outer aspect of the cardiac cell<br />
membranes (as for Ca 2 ). In addition, Mg 2 is a vasodilator<br />
<strong>and</strong> releases prostacyclin from damaged vascular tissue<br />
in vitro.<br />
Adverse effects <strong>and</strong> contraindications<br />
• Excessively high extracellular concentrations of Mg 2 can<br />
cause neuromuscular blockade. Magnesium chloride<br />
should be used with great caution in patients with renal<br />
impairment or hypotension, <strong>and</strong> in patients receiving<br />
drugs with neuromuscular blocking activity, including<br />
aminoglycoside antibiotics.<br />
• Mg 2 can cause AV block.<br />
Pharmacokinetics<br />
Magnesium salts are not well absorbed from the gastrointestinal<br />
tract, accounting for their efficacy as osmotic laxatives<br />
when given by mouth. Mg 2 is eliminated in the urine <strong>and</strong><br />
therapy with magnesium salts should be avoided or the dose<br />
reduced (<strong>and</strong> frequency of determination of plasma Mg 2<br />
concentration increased) in patients with glomerular filtration<br />
rates 20 mL/min.<br />
Drug interactions<br />
Magnesium salts form precipitates if they are mixed with<br />
sodium bicarbonate <strong>and</strong>, as with calcium chloride, magnesium<br />
salts should not be administered at the same time as sodium<br />
bicarbonate, or through the same line without an intervening<br />
saline flush. Hypermagnesaemia increases neuromuscular<br />
blockade caused by drugs with nicotinic-receptor-antagonist<br />
properties (e.g. pancuronium, aminoglycosides).<br />
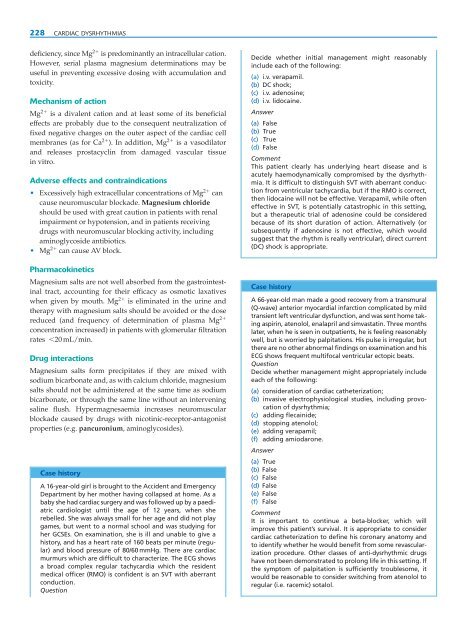
Case history<br />
A 16-year-old girl is brought to the Accident <strong>and</strong> Emergency<br />
Department by her mother having collapsed at home. As a<br />
baby she had cardiac surgery <strong>and</strong> was followed up by a paediatric<br />
cardiologist until the age of 12 years, when she<br />
rebelled. She was always small for her age <strong>and</strong> did not play<br />
games, but went to a normal school <strong>and</strong> was studying for<br />
her GCSEs. On examination, she is ill <strong>and</strong> unable to give a<br />
history, <strong>and</strong> has a heart rate of 160 beats per minute (regular)<br />
<strong>and</strong> blood pressure of 80/60 mmHg. There are cardiac<br />
murmurs which are difficult to characterize. The ECG shows<br />
a broad complex regular tachycardia which the resident<br />
medical officer (RMO) is confident is an SVT with aberrant<br />
conduction.<br />
Question<br />
Decide whether initial management might reasonably<br />
include each of the following:<br />
(a) i.v. verapamil.<br />
(b) DC shock;<br />
(c) i.v. adenosine;<br />
(d) i.v. lidocaine.<br />
Answer<br />
(a) False<br />
(b) True<br />
(c) True<br />
(d) False<br />
Comment<br />
This patient clearly has underlying heart disease <strong>and</strong> is<br />
acutely haemodynamically compromised by the dysrhythmia.<br />
It is difficult to distinguish SVT with aberrant conduction<br />
from ventricular tachycardia, but if the RMO is correct,<br />
then lidocaine will not be effective. Verapamil, while often<br />
effective in SVT, is potentially catastrophic in this setting,<br />
but a therapeutic trial of adenosine could be considered<br />
because of its short duration of action. Alternatively (or<br />
subsequently if adenosine is not effective, which would<br />
suggest that the rhythm is really ventricular), direct current<br />
(DC) shock is appropriate.<br />
Case history<br />
A 66-year-old man made a good recovery from a transmural<br />
(Q-wave) anterior myocardial infarction complicated by mild<br />
transient left ventricular dysfunction, <strong>and</strong> was sent home taking<br />
aspirin, atenolol, enalapril <strong>and</strong> simvastatin. Three months<br />
later, when he is seen in outpatients, he is feeling reasonably<br />
well, but is worried by palpitations. His pulse is irregular, but<br />
there are no other abnormal findings on examination <strong>and</strong> his<br />
ECG shows frequent multifocal ventricular ectopic beats.<br />
Question<br />
Decide whether management might appropriately include<br />
each of the following:<br />
(a) consideration of cardiac catheterization;<br />
(b) invasive electrophysiological studies, including provocation<br />
of dysrhythmia;<br />
(c) adding flecainide;<br />
(d) stopping atenolol;<br />
(e) adding verapamil;<br />
(f) adding amiodarone.<br />
Answer<br />
(a) True<br />
(b) False<br />
(c) False<br />
(d) False<br />
(e) False<br />
(f) False<br />
Comment<br />
It is important to continue a beta-blocker, which will<br />
improve this patient’s survival. It is appropriate to consider<br />
cardiac catheterization to define his coronary anatomy <strong>and</strong><br />
to identify whether he would benefit from some revascularization<br />
procedure. Other classes of anti-dysrhythmic drugs<br />
have not been demonstrated to prolong life in this setting. If<br />
the symptom of palpitation is sufficiently troublesome, it<br />
would be reasonable to consider switching from atenolol to<br />
regular (i.e. racemic) sotalol.