Hyperbaric Oxygen Therapy - Hyperbaric Chamber Information ...
Hyperbaric Oxygen Therapy - Hyperbaric Chamber Information ...
Hyperbaric Oxygen Therapy - Hyperbaric Chamber Information ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
HBOT used in conjunction with thrombolytic therapy may be beneficial in pain relief<br />
although more studies are needed to arrive at a firm and generalisable conclusion.<br />
Cerebrovascular disease<br />
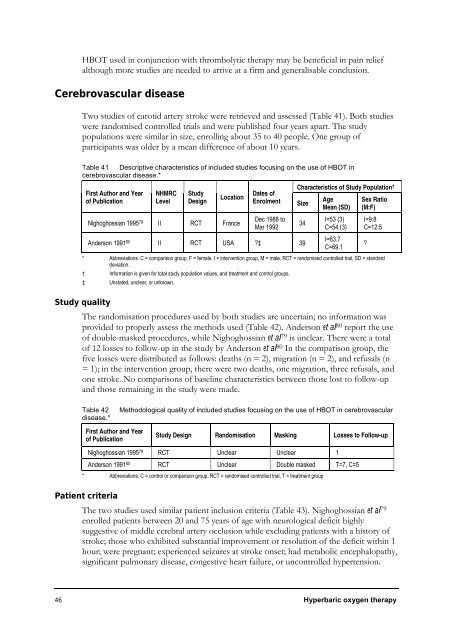
Two studies of carotid artery stroke were retrieved and assessed (Table 41). Both studies<br />
were randomised controlled trials and were published four years apart. The study<br />
populations were similar in size, enrolling about 35 to 40 people. One group of<br />
participants was older by a mean difference of about 10 years.<br />
Table 41 Descriptive characteristics of included studies focusing on the use of HBOT in<br />
cerebrovascular disease.*<br />
First Author and Year<br />
of Publication<br />
NHMRC<br />
Level<br />
Study<br />
Design<br />
Location<br />
Nighoghossian 1995 79 II RCT France<br />
Dates of<br />
Enrolment Size<br />
Dec 1988 to<br />
Mar 1992<br />
Anderson 1991 80 II RCT USA ?‡ 39<br />
Characteristics of Study Population †<br />
Age<br />
Mean (SD)<br />
Sex Ratio<br />
(M:F)<br />
46 <strong>Hyperbaric</strong> oxygen therapy<br />
34<br />
I=53 (3)<br />
C=54 (3)<br />
I=63.7<br />
C=69.1<br />
I=9:8<br />
C=12:5<br />
* Abbreviations: C = comparison group, F = female, I = intervention group, M = male, RCT = randomised controlled trial, SD = standard<br />
deviation.<br />
† <strong>Information</strong> is given for total study population values, and treatment and control groups.<br />
‡ Unstated, unclear, or unknown.<br />
Study quality<br />
The randomisation procedures used by both studies are uncertain; no information was<br />
provided to properly assess the methods used (Table 42). Anderson et al80 report the use<br />
of double-masked procedures, while Nighoghossian et al79 is unclear. There were a total<br />
of 12 losses to follow-up in the study by Anderson et al80 In the comparison group, the<br />
five losses were distributed as follows: deaths (n = 2), migration (n = 2), and refusals (n<br />
= 1); in the intervention group, there were two deaths, one migration, three refusals, and<br />
one stroke. No comparisons of baseline characteristics between those lost to follow-up<br />
and those remaining in the study were made.<br />
Table 42 Methodological quality of included studies focusing on the use of HBOT in cerebrovascular<br />
disease.*<br />
First Author and Year<br />
of Publication<br />
Study Design Randomisation Masking Losses to Follow-up<br />
Nighoghossian 1995 79 RCT Unclear Unclear 1<br />
Anderson 1991 80 RCT Unclear Double masked T=7, C=5<br />
* Abbreviations: C = control or comparison group, RCT = randomised controlled trial, T = treatment group<br />
Patient criteria<br />
The two studies used similar patient inclusion criteria (Table 43). Nighoghossian et al79 enrolled patients between 20 and 75 years of age with neurological deficit highly<br />
suggestive of middle cerebral artery occlusion while excluding patients with a history of<br />
stroke; those who exhibited substantial improvement or resolution of the deficit within 1<br />
hour; were pregnant; experienced seizures at stroke onset; had metabolic encephalopathy,<br />
significant pulmonary disease, congestive heart failure, or uncontrolled hypertension.<br />
?