- Page 1 and 2:
Lung Cancer Frank V. Fossella, MD R
- Page 3 and 4:
This page intentionally left blank
- Page 5 and 6:
Frank V. Fossella, MD Department of
- Page 7 and 8:
vi Foreword possible. Since the res
- Page 9 and 10:
This page intentionally left blank
- Page 11 and 12:
x Contents Chapter 7 Surgical Treat
- Page 13 and 14:
xii Contributors Joe B. Putnam, Jr.
- Page 15 and 16:
2 J.B. Putnam, Jr., F.V. Fossella,
- Page 17 and 18:
4 J.B. Putnam, Jr., F.V. Fossella,
- Page 19 and 20:
6 J.B. Putnam, Jr., F.V. Fossella,
- Page 21 and 22:
8 J.B. Putnam, Jr., F.V. Fossella,
- Page 23 and 24:
10 J.B. Putnam, Jr., F.V. Fossella,
- Page 25 and 26:
12 J.B. Putnam, Jr., F.V. Fossella,
- Page 27 and 28:
14 J.B. Putnam, Jr., F.V. Fossella,
- Page 29 and 30:
16 J.B. Putnam, Jr., F.V. Fossella,
- Page 31 and 32:
18 J.B. Putnam, Jr., F.V. Fossella,
- Page 33 and 34:
20 J.B. Putnam, Jr., F.V. Fossella,
- Page 35 and 36:
22 J.B. Putnam, Jr., F.V. Fossella,
- Page 37 and 38:
24 J.B. Putnam, Jr., F.V. Fossella,
- Page 39 and 40:
26 F.V. Fossella common sites of lu
- Page 41 and 42:
28 F.V. Fossella history and physic
- Page 43 and 44:
30 F.V. Fossella Computed Tomograph
- Page 45 and 46:
32 F.V. Fossella Pulmonary Function
- Page 47 and 48:
34 F.V. Fossella The use of flexibl
- Page 49 and 50:
36 R.F. Munden and J.J. Erasmus hav
- Page 51 and 52:
38 R.F. Munden and J.J. Erasmus che
- Page 53 and 54:
40 R.F. Munden and J.J. Erasmus tha
- Page 55 and 56:
42 R.F. Munden and J.J. Erasmus (Gu
- Page 57 and 58:
44 R.F. Munden and J.J. Erasmus A B
- Page 59 and 60: 46 R.F. Munden and J.J. Erasmus in
- Page 61 and 62: 48 R.F. Munden and J.J. Erasmus Pat
- Page 63 and 64: 50 R.F. Munden and J.J. Erasmus D C
- Page 65 and 66: 52 R.F. Munden and J.J. Erasmus A B
- Page 67 and 68: 54 R.F. Munden and J.J. Erasmus Bol
- Page 69 and 70: 56 R.F. Munden and J.J. Erasmus Swe
- Page 71 and 72: 58 P. Tamboli and J.Y. Ro Chapter O
- Page 73 and 74: 60 P. Tamboli and J.Y. Ro Figure 4-
- Page 75 and 76: 62 P. Tamboli and J.Y. Ro Postopera
- Page 77 and 78: 64 P. Tamboli and J.Y. Ro Table 4-1
- Page 79 and 80: 66 P. Tamboli and J.Y. Ro Atypical
- Page 81 and 82: 68 P. Tamboli and J.Y. Ro Diffuse I
- Page 83 and 84: 70 P. Tamboli and J.Y. Ro noma. Cig
- Page 85 and 86: 72 P. Tamboli and J.Y. Ro Figure 4-
- Page 87 and 88: 74 P. Tamboli and J.Y. Ro alone. BA
- Page 89 and 90: 76 P. Tamboli and J.Y. Ro Other Mal
- Page 91 and 92: 78 P. Tamboli and J.Y. Ro Electron
- Page 93 and 94: 80 P. Tamboli and J.Y. Ro Niho S, Y
- Page 95 and 96: 82 Y. De Jesus and G.L. Walsh Chapt
- Page 97 and 98: 84 Y. De Jesus and G.L. Walsh Figur
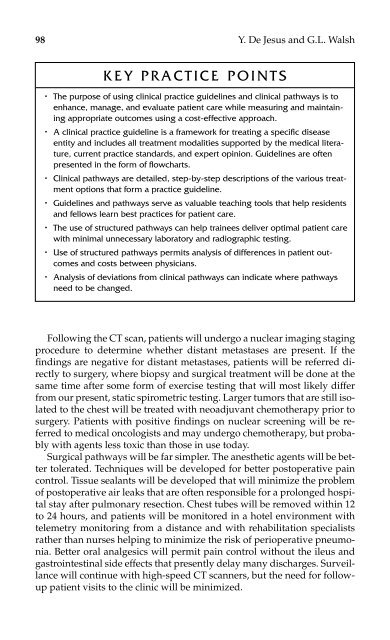
- Page 99 and 100: 86 Y. De Jesus and G.L. Walsh guide
- Page 101 and 102: 88 Y. De Jesus and G.L. Walsh with
- Page 103 and 104: Figure 5-2. Patient “pathway to r
- Page 105 and 106: 92 Y. De Jesus and G.L. Walsh Figur
- Page 107 and 108: 94 Y. De Jesus and G.L. Walsh Recov
- Page 109: 96 Y. De Jesus and G.L. Walsh Figur
- Page 113 and 114: 100 Y. De Jesus and G.L. Walsh Jenn
- Page 115 and 116: 102 W.R. Smythe nation for these su
- Page 117 and 118: 104 W.R. Smythe patient reports of
- Page 119 and 120: 106 W.R. Smythe bar or limited lung
- Page 121 and 122: 108 W.R. Smythe hospitals for 149 p
- Page 123 and 124: 110 W.R. Smythe Figure 6-1. Postsur
- Page 125 and 126: 112 W.R. Smythe nant neoplasms has
- Page 127 and 128: 114 W.R. Smythe Future Directions F
- Page 129 and 130: 116 W.R. Smythe Henschke CI, McCaul
- Page 131 and 132: 7 SURGICAL TREATMENT OF LOCALLY ADV
- Page 133 and 134: 120 S.G. Swisher Treatment Options
- Page 135 and 136: 122 S.G. Swisher Initial Assessment
- Page 137 and 138: 124 S.G. Swisher Figure 7-1. Region
- Page 139 and 140: 126 S.G. Swisher Table 7-2. (contin
- Page 141 and 142: 128 S.G. Swisher upper paratracheal
- Page 143 and 144: 130 S.G. Swisher is performed only
- Page 145 and 146: 132 S.G. Swisher chance for long-te
- Page 147 and 148: 134 S.G. Swisher Pancoast tumors th
- Page 149 and 150: 136 S.G. Swisher A B Figure 7-2. Do
- Page 151 and 152: 138 S.G. Swisher a combination of t
- Page 153 and 154: 140 S.G. Swisher Dartevelle PG, Cha
- Page 155 and 156: 8 NONSURGICAL TREATMENT OF EARLY-ST
- Page 157 and 158: 144 R. Komaki morbid conditions pre
- Page 159 and 160: 146 R. Komaki and 26 patients had c
- Page 161 and 162:
148 R. Komaki Around 1998, by using
- Page 163 and 164:
150 R. Komaki Table 8-5. Survival a
- Page 165 and 166:
152 R. Komaki A total of 610 patien
- Page 167 and 168:
154 R. Komaki tially obstructed air
- Page 169 and 170:
156 R. Komaki report of Radiation T
- Page 171 and 172:
9 TREATMENT OF PATIENTS WITH ADVANC
- Page 173 and 174:
160 R. Zinner chemotherapy, in pati
- Page 175 and 176:
Table 9-1. Chemotherapy in Older Pa
- Page 177 and 178:
164 R. Zinner results of additional
- Page 179 and 180:
Table 9-3. Third-Generation-Agent M
- Page 181 and 182:
Table 9-4. Third-Generation Agents
- Page 183 and 184:
Table 9-5. Third-Generation Platinu
- Page 185 and 186:
Table 9-6. Comparisons between Diff
- Page 187 and 188:
174 R. Zinner may play an important
- Page 189 and 190:
Table 9-8. Third-Generation Cisplat
- Page 191 and 192:
178 R. Zinner wards higher survival
- Page 193 and 194:
180 R. Zinner KEY PRACTICE POINTS
- Page 195 and 196:
182 R. Zinner DeVore RF, Fehrenbach
- Page 197 and 198:
184 R. Zinner Perng RP, Chen YM, Mi
- Page 199 and 200:
10 TREATMENT OF LIMITED-STAGE SMALL
- Page 201 and 202:
188 R. Komaki Age is not a signific
- Page 203 and 204:
190 R. Komaki lished between 1979 a
- Page 205 and 206:
Table 10-1. Complete Response Rates
- Page 207 and 208:
194 R. Komaki twice daily to a tota
- Page 209 and 210:
196 R. Komaki Intergroup study 0096
- Page 211 and 212:
198 R. Komaki Figure 10-1. Survival
- Page 213 and 214:
200 R. Komaki cisplatin with concur
- Page 215 and 216:
202 R. Komaki KEY PRACTICE POINTS
- Page 217 and 218:
204 R. Komaki tients (Pts) with lim
- Page 219 and 220:
206 R. Komaki Wagner H, Kim K, John
- Page 221 and 222:
208 G.R. Blumenschein, Jr. recurs a
- Page 223 and 224:
210 G.R. Blumenschein, Jr. syndrome
- Page 225 and 226:
212 G.R. Blumenschein, Jr. toxicity
- Page 227 and 228:
214 G.R. Blumenschein, Jr. the year
- Page 229 and 230:
216 G.R. Blumenschein, Jr. is chara
- Page 231 and 232:
218 G.R. Blumenschein, Jr. new cyto
- Page 233 and 234:
12 PALLIATIVE CARE IN PATIENTS WITH
- Page 235 and 236:
222 J.B. Putnam, Jr. therapy. Patie
- Page 237 and 238:
224 J.B. Putnam, Jr. tion—includi
- Page 239 and 240:
226 J.B. Putnam, Jr. rates were 47%
- Page 241 and 242:
228 J.B. Putnam, Jr. Dyspnea The ma
- Page 243 and 244:
230 J.B. Putnam, Jr. Small-bore cat
- Page 245 and 246:
232 J.B. Putnam, Jr. A B Figure 12-
- Page 247 and 248:
234 J.B. Putnam, Jr. C D Figure 12-
- Page 249 and 250:
236 J.B. Putnam, Jr. B Figure 12-3.
- Page 251 and 252:
238 J.B. Putnam, Jr. KEY PRACTICE P
- Page 253 and 254:
240 J.B. Putnam, Jr. Rendina EA, De
- Page 255 and 256:
242 A.A. Vaporciyan, J.F. Kelly, an
- Page 257 and 258:
244 A.A. Vaporciyan, J.F. Kelly, an
- Page 259 and 260:
246 A.A. Vaporciyan, J.F. Kelly, an
- Page 261 and 262:
248 A.A. Vaporciyan, J.F. Kelly, an
- Page 263 and 264:
250 A.A. Vaporciyan, J.F. Kelly, an
- Page 265 and 266:
252 A.A. Vaporciyan, J.F. Kelly, an
- Page 267 and 268:
254 A.A. Vaporciyan, J.F. Kelly, an
- Page 269 and 270:
14 PREVENTION AND EARLY DETECTION O
- Page 271 and 272:
258 E.S. Kim and F.R. Khuri A secon
- Page 273 and 274:
260 E.S. Kim and F.R. Khuri Smoking
- Page 275 and 276:
262 E.S. Kim and F.R. Khuri Reversa
- Page 277 and 278:
264 E.S. Kim and F.R. Khuri yet to
- Page 279 and 280:
266 E.S. Kim and F.R. Khuri nation
- Page 281 and 282:
268 E.S. Kim and F.R. Khuri Methodo
- Page 283 and 284:
270 E.S. Kim and F.R. Khuri have be
- Page 285 and 286:
272 E.S. Kim and F.R. Khuri the tre
- Page 287 and 288:
274 E.S. Kim and F.R. Khuri changes
- Page 289 and 290:
276 E.S. Kim and F.R. Khuri KEY PRA
- Page 291 and 292:
278 E.S. Kim and F.R. Khuri Hong WK
- Page 293 and 294:
15 MOLECULAR EVENTS IN LUNG CANCER
- Page 295 and 296:
282 W.N. Hittelman, J.M. Kurie, and
- Page 297 and 298:
284 W.N. Hittelman, J.M. Kurie, and
- Page 299 and 300:
286 W.N. Hittelman, J.M. Kurie, and
- Page 301 and 302:
288 W.N. Hittelman, J.M. Kurie, and
- Page 303 and 304:
290 W.N. Hittelman, J.M. Kurie, and
- Page 305 and 306:
292 W.N. Hittelman, J.M. Kurie, and
- Page 307 and 308:
294 W.N. Hittelman, J.M. Kurie, and
- Page 309 and 310:
296 W.N. Hittelman, J.M. Kurie, and
- Page 311 and 312:
298 W.N. Hittelman, J.M. Kurie, and
- Page 313 and 314:
300 Index Anterior spinal column re
- Page 315 and 316:
302 Index Cardiac murmurs, 104 Card
- Page 317 and 318:
304 Index Diagnosis. See also under
- Page 319 and 320:
306 Index Growth. See Tumor growth
- Page 321 and 322:
308 Index Magnetic resonance (MR) i
- Page 323 and 324:
310 Index p16 gene, 285 p19 arf gen
- Page 325 and 326:
312 Index Pulmonary resection (cont
- Page 327 and 328:
314 Index Squamous metaplasia, 263-
- Page 329:
316 Index Vitamin A, 262 Vocal cord