CHAPTER X CHAPTER 4 - Cancer et environnement
CHAPTER X CHAPTER 4 - Cancer et environnement
CHAPTER X CHAPTER 4 - Cancer et environnement
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
small tumour insufficient to produce a<br />
palpable or macroscopic mass or at the<br />
edge of a large tumour; intratubular infiltration;<br />
pag<strong>et</strong>oid spread along the r<strong>et</strong>e.<br />
Seminoma cells are round or polygonal<br />
with a distinct membrane. Cytoplasm is<br />
usually clear reflecting the glycogen or<br />
lipid content. Less commonly, they have<br />
more densely staining cytoplasm. Nuclei<br />
contain prominent nucleoli, which may<br />
be bar shaped. Mitoses are variable in<br />
number.<br />
A<br />
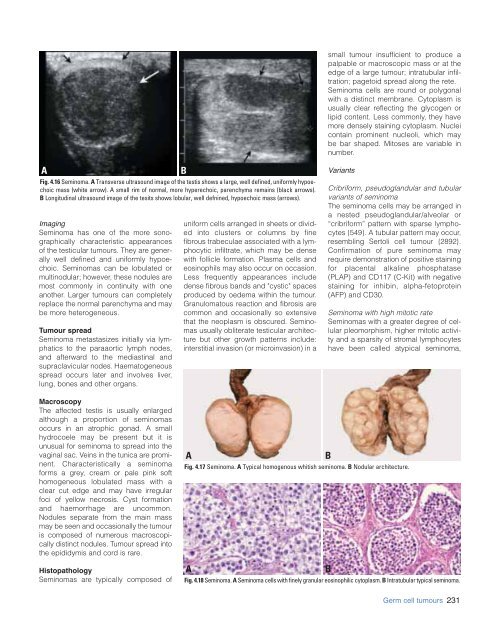
Fig. 4.16 Seminoma. A Transverse ultrasound image of the testis shows a large, well defined, uniformly hypoechoic<br />
mass (white arrow). A small rim of normal, more hyperechoic, parenchyma remains (black arrows).<br />
B Longitudinal ultrasound image of the tesits shows lobular, well defnined, hypoechoic mass (arrows).<br />
Imaging<br />
Seminoma has one of the more sonographically<br />
characteristic appearances<br />
of the testicular tumours. They are generally<br />
well defined and uniformly hypoechoic.<br />
Seminomas can be lobulated or<br />
multinodular; however, these nodules are<br />
most commonly in continuity with one<br />
another. Larger tumours can compl<strong>et</strong>ely<br />
replace the normal parenchyma and may<br />
be more h<strong>et</strong>erogeneous.<br />
Tumour spread<br />
Seminoma m<strong>et</strong>astasizes initially via lymphatics<br />
to the paraaortic lymph nodes,<br />
and afterward to the mediastinal and<br />
supraclavicular nodes. Haematogeneous<br />
spread occurs later and involves liver,<br />
lung, bones and other organs.<br />
B<br />
uniform cells arranged in she<strong>et</strong>s or divided<br />
into clusters or columns by fine<br />
fibrous trabeculae associated with a lymphocytic<br />
infiltrate, which may be dense<br />
with follicle formation. Plasma cells and<br />
eosinophils may also occur on occasion.<br />
Less frequently appearances include<br />
dense fibrous bands and "cystic" spaces<br />
produced by oedema within the tumour.<br />
Granulomatous reaction and fibrosis are<br />
common and occasionally so extensive<br />
that the neoplasm is obscured. Seminomas<br />
usually obliterate testicular architecture<br />
but other growth patterns include:<br />
interstitial invasion (or microinvasion) in a<br />
Variants<br />
Cribriform, pseudoglandular and tubular<br />
variants of seminoma<br />
The seminoma cells may be arranged in<br />
a nested pseudoglandular/alveolar or<br />
“cribriform” pattern with sparse lymphocytes<br />
{549}. A tubular pattern may occur,<br />
resembling Sertoli cell tumour {2892}.<br />
Confirmation of pure seminoma may<br />
require demonstration of positive staining<br />
for placental alkaline phosphatase<br />
(PLAP) and CD117 (C-Kit) with negative<br />
staining for inhibin, alpha-f<strong>et</strong>oprotein<br />
(AFP) and CD30.<br />
Seminoma with high mitotic rate<br />
Seminomas with a greater degree of cellular<br />
pleomorphism, higher mitotic activity<br />
and a sparsity of stromal lymphocytes<br />
have been called atypical seminoma,<br />
Macroscopy<br />
The affected testis is usually enlarged<br />
although a proportion of seminomas<br />
occurs in an atrophic gonad. A small<br />
hydrocoele may be present but it is<br />
unusual for seminoma to spread into the<br />
vaginal sac. Veins in the tunica are prominent.<br />
Characteristically a seminoma<br />
forms a grey, cream or pale pink soft<br />
homogeneous lobulated mass with a<br />
clear cut edge and may have irregular<br />
foci of yellow necrosis. Cyst formation<br />
and haemorrhage are uncommon.<br />
Nodules separate from the main mass<br />
may be seen and occasionally the tumour<br />
is composed of numerous macroscopically<br />
distinct nodules. Tumour spread into<br />
the epididymis and cord is rare.<br />
Histopathology<br />
Seminomas are typically composed of<br />
A<br />
B<br />
Fig. 4.17 Seminoma. A Typical homogenous whitish seminoma. B Nodular architecture.<br />
A<br />
B<br />
Fig. 4.18 Seminoma. A Seminoma cells with finely granular eosinophilic cytoplasm. B Intratubular typical seminoma.<br />
Germ cell tumours 231