A-Textbook-of-Clinical-Pharmacology-and-Therapeutics-5th-edition
A-Textbook-of-Clinical-Pharmacology-and-Therapeutics-5th-edition
A-Textbook-of-Clinical-Pharmacology-and-Therapeutics-5th-edition
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
SCHIZOPHRENIA 111<br />
Box 19.1: Dopamine theory <strong>of</strong> schizophrenia<br />
• There is excess dopamine activity in the mesolimbic<br />
system in schizophrenia.<br />
• Antipsychotic potency is <strong>of</strong>ten proportional to<br />
D 2 -blocking potency.<br />
• Amphetamine (which increases dopamine release) can<br />
produce acute psychosis that is indistinguishable from<br />
acute schizophrenia (positive symptoms).<br />
• D 2 agonists (bromocriptine <strong>and</strong> apomorphine)<br />
aggravate schizophrenia in schizophrenic patients.<br />
• There is an increase in D 2 <strong>and</strong> D 4 receptors on PET in<br />
schizophrenic patients.<br />
• L-Dopa can cause hallucinations <strong>and</strong> acute psychotic<br />
reactions <strong>and</strong> paranoia, but does not cause all the<br />
features <strong>of</strong> these conditions.<br />
• There is no definite increase in brain dopamine in vivo<br />
<strong>and</strong> post mortem.<br />
• Dopamine receptor blockade does not fully alleviate<br />
symptoms.<br />
Box 19.2: 5-Hydroxytryptamine <strong>and</strong> schizophrenia<br />
• LSD acts on 5HT receptors, causing hallucinations <strong>and</strong><br />
dramatic psychological effects which may mimic some<br />
features <strong>of</strong> schizophrenia.<br />
• 5HT has a modulatory effect on dopamine pathways.<br />
• Many effective antipsychotic drugs have dopamine <strong>and</strong><br />
5HT 2 receptor-blocking properties.<br />
• 5HT 2 receptor blockade is not essential for drug efficacy.<br />
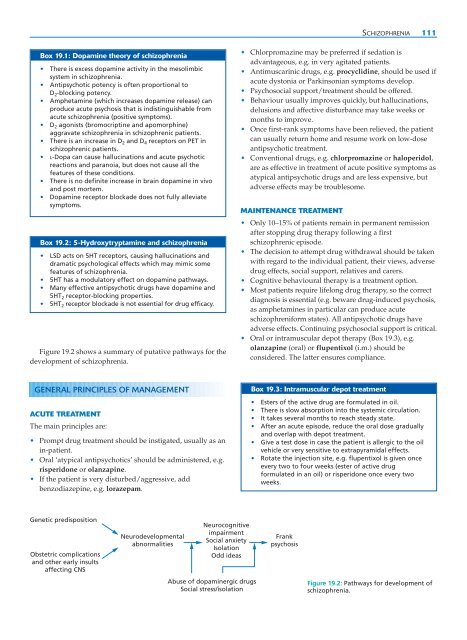
Figure 19.2 shows a summary <strong>of</strong> putative pathways for the<br />
development <strong>of</strong> schizophrenia.<br />
• Chlorpromazine may be preferred if sedation is<br />
advantageous, e.g. in very agitated patients.<br />
• Antimuscarinic drugs, e.g. procyclidine, should be used if<br />
acute dystonia or Parkinsonian symptoms develop.<br />
• Psychosocial support/treatment should be <strong>of</strong>fered.<br />
• Behaviour usually improves quickly, but hallucinations,<br />
delusions <strong>and</strong> affective disturbance may take weeks or<br />
months to improve.<br />
• Once first-rank symptoms have been relieved, the patient<br />
can usually return home <strong>and</strong> resume work on low-dose<br />
antipsychotic treatment.<br />
• Conventional drugs, e.g. chlorpromazine or haloperidol,<br />
are as effective in treatment <strong>of</strong> acute positive symptoms as<br />
atypical antipsychotic drugs <strong>and</strong> are less expensive, but<br />
adverse effects may be troublesome.<br />
MAINTENANCE TREATMENT<br />
• Only 10–15% <strong>of</strong> patients remain in permanent remission<br />
after stopping drug therapy following a first<br />
schizophrenic episode.<br />
• The decision to attempt drug withdrawal should be taken<br />
with regard to the individual patient, their views, adverse<br />
drug effects, social support, relatives <strong>and</strong> carers.<br />
• Cognitive behavioural therapy is a treatment option.<br />
• Most patients require lifelong drug therapy, so the correct<br />
diagnosis is essential (e.g. beware drug-induced psychosis,<br />
as amphetamines in particular can produce acute<br />
schizophreniform states). All antipsychotic drugs have<br />
adverse effects. Continuing psychosocial support is critical.<br />
• Oral or intramuscular depot therapy (Box 19.3), e.g.<br />
olanzapine (oral) or flupentixol (i.m.) should be<br />
considered. The latter ensures compliance.<br />
GENERAL PRINCIPLES OF MANAGEMENT<br />
ACUTE TREATMENT<br />
The main principles are:<br />
• Prompt drug treatment should be instigated, usually as an<br />
in-patient.<br />
• Oral ‘atypical antipsychotics’ should be administered, e.g.<br />
risperidone or olanzapine.<br />
• If the patient is very disturbed/aggressive, add<br />
benzodiazepine, e.g. lorazepam.<br />
Box 19.3: Intramuscular depot treatment<br />
• Esters <strong>of</strong> the active drug are formulated in oil.<br />
• There is slow absorption into the systemic circulation.<br />
• It takes several months to reach steady state.<br />
• After an acute episode, reduce the oral dose gradually<br />
<strong>and</strong> overlap with depot treatment.<br />
• Give a test dose in case the patient is allergic to the oil<br />
vehicle or very sensitive to extrapyramidal effects.<br />
• Rotate the injection site, e.g. flupentixol is given once<br />
every two to four weeks (ester <strong>of</strong> active drug<br />
formulated in an oil) or risperidone once every two<br />
weeks.<br />
Genetic predisposition<br />
Obstetric complications<br />
<strong>and</strong> other early insults<br />
affecting CNS<br />
Neurodevelopmental<br />
abnormalities<br />
Neurocognitive<br />
impairment<br />
Social anxiety<br />
Isolation<br />
Odd ideas<br />
Frank<br />
psychosis<br />
Abuse <strong>of</strong> dopaminergic drugs<br />
Social stress/isolation<br />
Figure 19.2: Pathways for development <strong>of</strong><br />
schizophrenia.