A-Textbook-of-Clinical-Pharmacology-and-Therapeutics-5th-edition
A-Textbook-of-Clinical-Pharmacology-and-Therapeutics-5th-edition
A-Textbook-of-Clinical-Pharmacology-and-Therapeutics-5th-edition
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
36 EFFECTS OF DISEASE ON DRUG DISPOSITION<br />
<strong>and</strong> other plasma proteins. This alters the pharmacokinetics <strong>of</strong><br />
many drugs, but is seldom clinically important. Phenytoin<br />
is an exception, because therapy is guided by plasma concentration<br />
<strong>and</strong> routine analytical methods detect total (bound<br />
<strong>and</strong> free) drug. In renal impairment, phenytoin protein binding<br />
is reduced by competition with accumulated molecules<br />
normally cleared by the kidney <strong>and</strong> which bind to the same<br />
albumin drug-binding site as phenytoin. Thus, for any measured<br />
phenytoin concentration, free (active) drug is increased<br />
compared to a subject with normal renal function <strong>and</strong> the<br />
same measured total concentration. The therapeutic range<br />
therefore has to be adjusted to lower values in patients with<br />
renal impairment, as otherwise doses will be selected that<br />
cause toxicity.<br />
Tissue binding <strong>of</strong> digoxin is reduced in patients with<br />
impaired renal function, resulting in a lower volume <strong>of</strong> distribution<br />
than in healthy subjects. A reduced loading dose <strong>of</strong><br />
digoxin is therefore appropriate in such patients, although the<br />
effect <strong>of</strong> reduced glomerular filtration on digoxin clearance is<br />
even more important, necessitating a reduced maintenance<br />
dose, as described below.<br />
The blood–brain barrier is more permeable to drugs in<br />
uraemia. This can result in increased access <strong>of</strong> drugs to the<br />
central nervous system, an effect that is believed to contribute<br />
to the increased incidence <strong>of</strong> confusion caused by cimetidine,<br />
ranitidine <strong>and</strong> famotidine in patients with renal failure.<br />
METABOLISM<br />
Metabolism <strong>of</strong> several drugs is reduced in renal failure. These<br />
include drugs that undergo phase I metabolism by CYP3A4.<br />
Drugs that are mainly metabolized by phase II drug metabolism<br />
are less affected, although conversion <strong>of</strong> sulindac to its<br />
active sulphide metabolite is impaired in renal failure, as is the<br />
hepatic conjugation <strong>of</strong> metoclopramide with glucuronide <strong>and</strong><br />
sulphate.<br />
RENAL EXCRETION<br />
Glomerular filtration <strong>and</strong> tubular secretion <strong>of</strong> drugs usually<br />
fall in step with one another in patients with renal impairment.<br />
Drug excretion is directly related to glomerular filtration<br />
rate (GFR). Some estimate <strong>of</strong> GFR (eGFR) is therefore<br />
essential when deciding on an appropriate dose regimen.<br />
Serum creatinine concentration adjusted for age permits calculation<br />
<strong>of</strong> an estimate <strong>of</strong> GFR per 1.73 m 2 body surface area.<br />
This is now provided by most chemical pathology laboratories,<br />
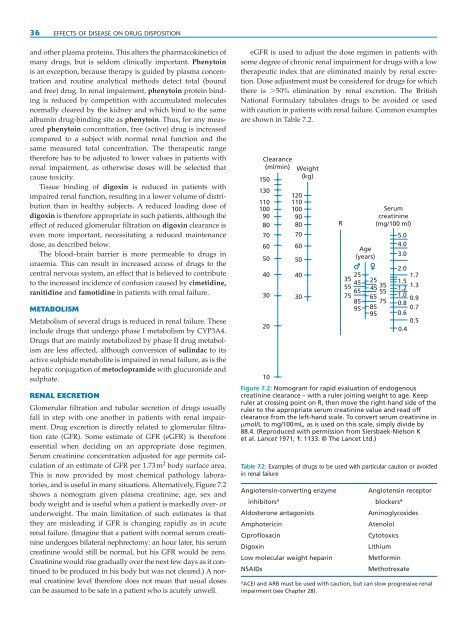
<strong>and</strong> is useful in many situations. Alternatively, Figure 7.2<br />
shows a nomogram given plasma creatinine, age, sex <strong>and</strong><br />
body weight <strong>and</strong> is useful when a patient is markedly over- or<br />
underweight. The main limitation <strong>of</strong> such estimates is that<br />
they are misleading if GFR is changing rapidly as in acute<br />
renal failure. (Imagine that a patient with normal serum creatinine<br />
undergoes bilateral nephrectomy: an hour later, his serum<br />
creatinine would still be normal, but his GFR would be zero.<br />
Creatinine would rise gradually over the next few days as it continued<br />
to be produced in his body but was not cleared.) A normal<br />
creatinine level therefore does not mean that usual doses<br />
can be assumed to be safe in a patient who is acutely unwell.<br />
eGFR is used to adjust the dose regimen in patients with<br />
some degree <strong>of</strong> chronic renal impairment for drugs with a low<br />
therapeutic index that are eliminated mainly by renal excretion.<br />
Dose adjustment must be considered for drugs for which<br />
there is 50% elimination by renal excretion. The British<br />
National Formulary tabulates drugs to be avoided or used<br />
with caution in patients with renal failure. Common examples<br />
are shown in Table 7.2.<br />
Clearance<br />
(ml/min)<br />
150<br />
130<br />
110<br />
100<br />
90<br />
80<br />
70<br />
60<br />
50<br />
40<br />
30<br />
20<br />
Weight<br />
(kg)<br />
120<br />
110<br />
100<br />
90<br />
80<br />
70<br />
60<br />
50<br />
40<br />
30<br />
R<br />
Age<br />
(years)<br />
25<br />
35<br />
45<br />
25<br />
55<br />
65<br />
45<br />
35<br />
55<br />
75 65<br />
85 75<br />
95 85<br />
95<br />
Serum<br />
creatinine<br />
(mg/100 ml)<br />
5.0<br />
4.0<br />
3.0<br />
2.0<br />
1.7<br />
1.5<br />
1.2<br />
1.3<br />
1.0<br />
0.9<br />
0.8 0.7<br />
0.6<br />
0.5<br />
0.4<br />
10<br />
Figure 7.2: Nomogram for rapid evaluation <strong>of</strong> endogenous<br />
creatinine clearance – with a ruler joining weight to age. Keep<br />
ruler at crossing point on R, then move the right-h<strong>and</strong> side <strong>of</strong> the<br />
ruler to the appropriate serum creatinine value <strong>and</strong> read <strong>of</strong>f<br />
clearance from the left-h<strong>and</strong> scale. To convert serum creatinine in<br />
mol/L to mg/100mL, as is used on this scale, simply divide by<br />
88.4. (Reproduced with permission from Siersbaek-Nielson K<br />
et al. Lancet 1971; 1: 1133. © The Lancet Ltd.)<br />
Table 7.2: Examples <strong>of</strong> drugs to be used with particular caution or avoided<br />
in renal failure<br />
Angiotensin-converting enzyme<br />
inhibitors a<br />
Aldosterone antagonists<br />
Amphotericin<br />
Cipr<strong>of</strong>loxacin<br />
Digoxin<br />
Low molecular weight heparin<br />
NSAIDs<br />
Angiotensin receptor<br />
blockers a<br />
Aminoglycosides<br />
Atenolol<br />
Cytotoxics<br />
Lithium<br />
Metformin<br />
Methotrexate<br />
a ACEI <strong>and</strong> ARB must be used with caution, but can slow progressive renal<br />
impairment (see Chapter 28).