A-Textbook-of-Clinical-Pharmacology-and-Therapeutics-5th-edition
A-Textbook-of-Clinical-Pharmacology-and-Therapeutics-5th-edition
A-Textbook-of-Clinical-Pharmacology-and-Therapeutics-5th-edition
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
ALZHEIMER’S DISEASE 131<br />
Cholinergic crisis<br />
Treatment <strong>of</strong> myasthenia with anticholinesterases can be usefully<br />
monitored clinically by observation <strong>of</strong> the pupil (a diameter<br />
<strong>of</strong> 2 mm or less in normal lighting suggests overdose).<br />
Overdosage produces a cholinergic crisis, <strong>and</strong> further drug<br />
should be withheld.<br />
ALZHEIMER’S DISEASE<br />
Alzheimer’s disease (AD) is the most common cause <strong>of</strong> dementia.<br />
Its incidence increases with age. It is estimated that approximately<br />
500 000 people in the USA are affected. The symptoms<br />
<strong>of</strong> Alzheimer’s disease are progressive memory impairment<br />
associated with a decline in language, visuospatial function,<br />
calculation <strong>and</strong> judgement. Ultimately, this leads to major<br />
behavioural <strong>and</strong> functional disability. Acetylcholinesterase<br />
inhibiting drugs, e.g. donepezil, can slow down the progression<br />
<strong>of</strong> mild <strong>and</strong> moderate Alzheimer’s disease, but the benefit<br />
is pitifully small <strong>and</strong> only temporary. <strong>Clinical</strong> trials <strong>of</strong> other<br />
drug therapy, such as oestrogens, non-steroidal anti-inflammatory<br />
drugs (NSAIDs), statins, metal chelation <strong>and</strong> vitamin E,<br />
have failed to show conclusive benefit. Depression is commonly<br />
associated with Alzheimer’s disease <strong>and</strong> can be treated<br />
with a selective serotonin reuptake inhibitor (SSRI), e.g. sertraline.<br />
Antipsychotic drugs <strong>and</strong> benzodiazepines are sometimes<br />
indicated in demented patients for symptoms <strong>of</strong> psychosis<br />
or agitation but their use is associated with an increased risk<br />
<strong>of</strong> stroke.<br />
PATHOPHYSIOLOGY<br />
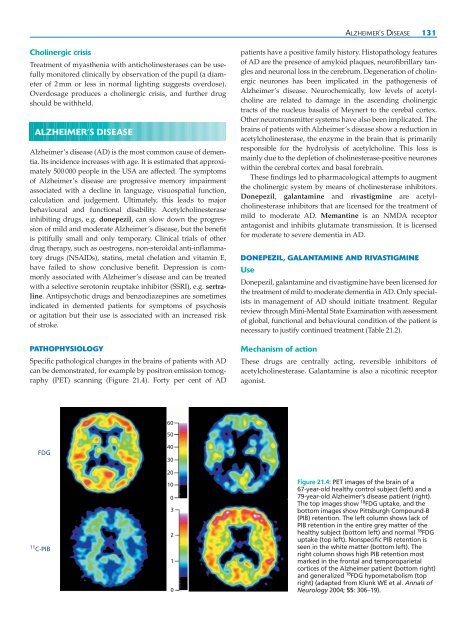
Specific pathological changes in the brains <strong>of</strong> patients with AD<br />
can be demonstrated, for example by positron emission tomography<br />
(PET) scanning (Figure 21.4). Forty per cent <strong>of</strong> AD<br />
patients have a positive family history. Histopathology features<br />
<strong>of</strong> AD are the presence <strong>of</strong> amyloid plaques, neur<strong>of</strong>ibrillary tangles<br />
<strong>and</strong> neuronal loss in the cerebrum. Degeneration <strong>of</strong> cholinergic<br />
neurones has been implicated in the pathogenesis <strong>of</strong><br />
Alzheimer’s disease. Neurochemically, low levels <strong>of</strong> acetylcholine<br />
are related to damage in the ascending cholinergic<br />
tracts <strong>of</strong> the nucleus basalis <strong>of</strong> Meynert to the cerebal cortex.<br />
Other neurotransmitter systems have also been implicated. The<br />
brains <strong>of</strong> patients with Alzheimer’s disease show a reduction in<br />
acetylcholinesterase, the enzyme in the brain that is primarily<br />
responsible for the hydrolysis <strong>of</strong> acetylcholine. This loss is<br />
mainly due to the depletion <strong>of</strong> cholinesterase-positive neurones<br />
within the cerebral cortex <strong>and</strong> basal forebrain.<br />
These findings led to pharmacological attempts to augment<br />
the cholinergic system by means <strong>of</strong> cholinesterase inhibitors.<br />
Donepezil, galantamine <strong>and</strong> rivastigmine are acetylcholinesterase<br />
inhibitors that are licensed for the treatment <strong>of</strong><br />
mild to moderate AD. Memantine is an NMDA receptor<br />
antagonist <strong>and</strong> inhibits glutamate transmission. It is licensed<br />
for moderate to severe dementia in AD.<br />
DONEPEZIL, GALANTAMINE AND RIVASTIGMINE<br />
Use<br />
Donepezil, galantamine <strong>and</strong> rivastigmine have been licensed for<br />
the treatment <strong>of</strong> mild to moderate dementia in AD. Only specialists<br />
in management <strong>of</strong> AD should initiate treatment. Regular<br />
review through Mini-Mental State Examination with assessment<br />
<strong>of</strong> global, functional <strong>and</strong> behavioural condition <strong>of</strong> the patient is<br />
necessary to justify continued treatment (Table 21.2).<br />
Mechanism <strong>of</strong> action<br />
These drugs are centrally acting, reversible inhibitors <strong>of</strong><br />
acetylcholinesterase. Galantamine is also a nicotinic receptor<br />
agonist.<br />
60<br />
50<br />
FDG<br />
11 C-PIB<br />
40<br />
30<br />
20<br />
10<br />
0<br />
3<br />
2<br />
1<br />
0<br />
Figure 21.4: PET images <strong>of</strong> the brain <strong>of</strong> a<br />
67-year-old healthy control subject (left) <strong>and</strong> a<br />
79-year-old Alzheimer’s disease patient (right).<br />
The top images show 18 FDG uptake, <strong>and</strong> the<br />
bottom images show Pittsburgh Compound-B<br />
(PIB) retention. The left column shows lack <strong>of</strong><br />
PIB retention in the entire grey matter <strong>of</strong> the<br />
healthy subject (bottom left) <strong>and</strong> normal 18 FDG<br />
uptake (top left). Nonspecific PIB retention is<br />
seen in the white matter (bottom left). The<br />
right column shows high PIB retention most<br />
marked in the frontal <strong>and</strong> temporoparietal<br />
cortices <strong>of</strong> the Alzheimer patient (bottom right)<br />
<strong>and</strong> generalized 18 FDG hypometabolism (top<br />
right) (adapted from Klunk WE et al. Annals <strong>of</strong><br />
Neurology 2004; 55: 306–19).