A-Textbook-of-Clinical-Pharmacology-and-Therapeutics-5th-edition
A-Textbook-of-Clinical-Pharmacology-and-Therapeutics-5th-edition
A-Textbook-of-Clinical-Pharmacology-and-Therapeutics-5th-edition
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
84 PHARMACOGENETICS<br />
for Ry1R or undergo muscle biopsy to assess their predisposition<br />
to this condition. Muscle from affected individuals is<br />
abnormally sensitive to caffeine in vitro, responding with a<br />
strong contraction to low concentrations. (Pharmacological<br />
doses <strong>of</strong> caffeine release calcium from intracellular stores<br />
<strong>and</strong> cause contraction even in normal muscle at sufficiently<br />
high concentration.) Affected muscle responds similarly to<br />
halothane or suxamethonium.<br />
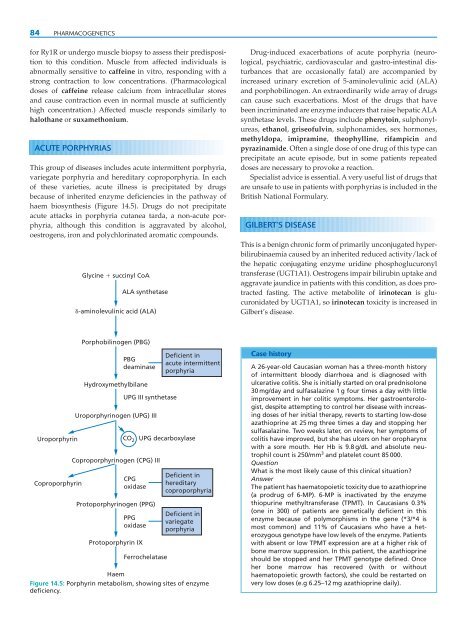
ACUTE PORPHYRIAS<br />
This group <strong>of</strong> diseases includes acute intermittent porphyria,<br />
variegate porphyria <strong>and</strong> hereditary coproporphyria. In each<br />
<strong>of</strong> these varieties, acute illness is precipitated by drugs<br />
because <strong>of</strong> inherited enzyme deficiencies in the pathway <strong>of</strong><br />
haem biosynthesis (Figure 14.5). Drugs do not precipitate<br />
acute attacks in porphyria cutanea tarda, a non-acute porphyria,<br />
although this condition is aggravated by alcohol,<br />
oestrogens, iron <strong>and</strong> polychlorinated aromatic compounds.<br />
Glycine succinyl CoA<br />
ALA synthetase<br />
-aminolevulinic acid (ALA)<br />
Drug-induced exacerbations <strong>of</strong> acute porphyria (neurological,<br />
psychiatric, cardiovascular <strong>and</strong> gastro-intestinal disturbances<br />
that are occasionally fatal) are accompanied by<br />
increased urinary excretion <strong>of</strong> 5-aminolevulinic acid (ALA)<br />
<strong>and</strong> porphobilinogen. An extraordinarily wide array <strong>of</strong> drugs<br />
can cause such exacerbations. Most <strong>of</strong> the drugs that have<br />
been incriminated are enzyme inducers that raise hepatic ALA<br />
synthetase levels. These drugs include phenytoin, sulphonylureas,<br />
ethanol, grise<strong>of</strong>ulvin, sulphonamides, sex hormones,<br />
methyldopa, imipramine, theophylline, rifampicin <strong>and</strong><br />
pyrazinamide. Often a single dose <strong>of</strong> one drug <strong>of</strong> this type can<br />
precipitate an acute episode, but in some patients repeated<br />
doses are necessary to provoke a reaction.<br />
Specialist advice is essential. A very useful list <strong>of</strong> drugs that<br />
are unsafe to use in patients with porphyrias is included in the<br />
British National Formulary.<br />
GILBERT’S DISEASE<br />
This is a benign chronic form <strong>of</strong> primarily unconjugated hyperbilirubinaemia<br />
caused by an inherited reduced activity/lack <strong>of</strong><br />
the hepatic conjugating enzyme uridine phosphoglucuronyl<br />
transferase (UGT1A1). Oestrogens impair bilirubin uptake <strong>and</strong><br />
aggravate jaundice in patients with this condition, as does protracted<br />
fasting. The active metabolite <strong>of</strong> irinotecan is glucuronidated<br />
by UGT1A1, so irinotecan toxicity is increased in<br />
Gilbert’s disease.<br />
Porphobilinogen (PBG)<br />
Uroporphyrin<br />
Coproporphyrin<br />
PBG<br />
deaminase<br />
Hydroxymethylbilane<br />
UPG III synthetase<br />
Uroporphyrinogen (UPG) III<br />
CO 2<br />
Coproporphyrinogen (CPG) III<br />
CPG<br />
oxidase<br />
Protoporphyrinogen (PPG)<br />
PPG<br />
oxidase<br />
Protoporphyrin IX<br />
UPG decarboxylase<br />
Ferrochelatase<br />
Deficient in<br />
acute intermittent<br />
porphyria<br />
Deficient in<br />
hereditary<br />
coproporphyria<br />
Deficient in<br />
variegate<br />
porphyria<br />
Haem<br />
Figure 14.5: Porphyrin metabolism, showing sites <strong>of</strong> enzyme<br />
deficiency.<br />
Case history<br />
A 26-year-old Caucasian woman has a three-month history<br />
<strong>of</strong> intermittent bloody diarrhoea <strong>and</strong> is diagnosed with<br />
ulcerative colitis. She is initially started on oral prednisolone<br />
30 mg/day <strong>and</strong> sulfasalazine 1 g four times a day with little<br />
improvement in her colitic symptoms. Her gastroenterologist,<br />
despite attempting to control her disease with increasing<br />
doses <strong>of</strong> her initial therapy, reverts to starting low-dose<br />
azathioprine at 25 mg three times a day <strong>and</strong> stopping her<br />
sulfasalazine. Two weeks later, on review, her symptoms <strong>of</strong><br />
colitis have improved, but she has ulcers on her oropharynx<br />
with a sore mouth. Her Hb is 9.8 g/dL <strong>and</strong> absolute neutrophil<br />
count is 250/mm 3 <strong>and</strong> platelet count 85 000.<br />
Question<br />
What is the most likely cause <strong>of</strong> this clinical situation<br />
Answer<br />
The patient has haematopoietic toxicity due to azathioprine<br />
(a prodrug <strong>of</strong> 6-MP). 6-MP is inactivated by the enzyme<br />
thiopurine methyltransferase (TPMT). In Caucasians 0.3%<br />
(one in 300) <strong>of</strong> patients are genetically deficient in this<br />
enzyme because <strong>of</strong> polymorphisms in the gene (*3/*4 is<br />
most common) <strong>and</strong> 11% <strong>of</strong> Caucasians who have a heterozygous<br />
genotype have low levels <strong>of</strong> the enzyme. Patients<br />
with absent or low TPMT expression are at a higher risk <strong>of</strong><br />
bone marrow suppression. In this patient, the azathioprine<br />
should be stopped <strong>and</strong> her TPMT genotype defined. Once<br />
her bone marrow has recovered (with or without<br />
haematopoietic growth factors), she could be restarted on<br />
very low doses (e.g 6.25–12 mg azathioprine daily).