A-Textbook-of-Clinical-Pharmacology-and-Therapeutics-5th-edition
A-Textbook-of-Clinical-Pharmacology-and-Therapeutics-5th-edition
A-Textbook-of-Clinical-Pharmacology-and-Therapeutics-5th-edition
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
364 MALARIA AND OTHER PARASITIC INFECTIONS<br />
8-AMINOQUINOLINES (PRIMAQUINE)<br />
Primaquine is used to eradicate the hepatic forms <strong>of</strong> P. vivax or<br />
P. malariae after st<strong>and</strong>ard chloroquine therapy, provided that the<br />
risk <strong>of</strong> re-exposure is low. It may also be used prophylactically<br />
with chloroquine. It interferes with the organism’s mitochondrial<br />
electron transport chain. Gastro-intestinal absorption is<br />
good <strong>and</strong> it is rapidly metabolized, with a mean t 1/2 <strong>of</strong> six<br />
hours. Its major adverse effects are gastro-intestinal upsets,<br />
methaemoglobinaemia <strong>and</strong> haemolytic anaemia in G6PDdeficient<br />
individuals.<br />
ARTENUSATE AND ARTEMETHER<br />
Uses<br />
Artemisinin (derived from the weed Quin Hao, Artemesia annua)<br />
is a sesquiterpene lactone endoperoxide. It has been used in<br />
China for at least 2000 years. Artenusate <strong>and</strong> artemether are<br />
semi-synthetic derivatives <strong>of</strong> artemisinin <strong>and</strong> are effective <strong>and</strong><br />
well-tolerated antimalarials. They should not be used as<br />
monotherapy or for prophylaxis because <strong>of</strong> the risk <strong>of</strong> resistance<br />
developing. In many developed countries, artemisinin derivatives<br />
are not yet licensed <strong>and</strong> can only be used on a namedpatient<br />
basis. Currently, there is no clinical evidence <strong>of</strong> resistance<br />
to artemesinin derivatives. Treatment can be started i.v. <strong>and</strong><br />
switched to oral with adjunctive doxycycline or clindamycin as<br />
with quinine.<br />
Mechanism <strong>of</strong> action<br />
Artemesinins undergo haem-mediated decomposition <strong>of</strong> the<br />
endoperoxide bridge to yield carbon-centred free radicals. The<br />
involvement <strong>of</strong> haem explains why they are selectively toxic to<br />
malaria parasites. The resulting carbon-centred free radicals<br />
alkylate haem <strong>and</strong> proteins, particularly in the membranes <strong>of</strong> the<br />
parasite’s food vacuole <strong>and</strong> mitochondria, causing rapid death.<br />
Adverse effects<br />
Side effects are mild <strong>and</strong> include the following:<br />
• nausea, vomiting <strong>and</strong> anorexia;<br />
• dizziness.<br />
Preclinical toxicology suggested neuro-, hepato- <strong>and</strong> bone<br />
marrow toxicity.<br />
Pharmacokinetics<br />
Oral absorption is fair (F 0.3). Artenusate <strong>and</strong> artemether<br />
reach peak plasma concentration in minutes <strong>and</strong> two to six<br />
hours, respectively. Both are extensively metabolized to dihydroartemesinin<br />
(active metabolite) which has a half-life <strong>of</strong><br />
one to two hours. They autoinduce their CYP450 catalysed<br />
metabolism. Drug–drug interactions are still being elucidated.<br />
ANTI-FOLATES (DAPSONE PROGUANIL,<br />
PYRIMETHAMINE)<br />
Combinations <strong>of</strong> these drugs are taken orally in malaria<br />
prophylaxis, but their efficacy in acute malaria treatment is<br />
limited due to resistance. These agents inhibit folate biosynthesis<br />
at all stages <strong>of</strong> the malaria parasite’s life cycle, acting<br />
as competitive inhibitors <strong>of</strong> the malarial dihydropteroate<br />
synthase (dapsone) or the malarial dihydr<strong>of</strong>olate reductase<br />
(proguanil or pyrimethamine). They exhibit typical anti-folate<br />
adverse effect pr<strong>of</strong>iles (gastro-intestinal upsets, skin rashes,<br />
myelosuppression; see Chapters 43 <strong>and</strong> 46).<br />
TREATMENT OF A MALARIA RELAPSE<br />
Plasmodium falciparum does not cause a relapsing illness after<br />
treating the acute attack with schizonticides, because there is no<br />
persistent liver stage <strong>of</strong> the parasite. Infections with P. malariae<br />
can cause recurrent attacks <strong>of</strong> fever for up to 30 years, but st<strong>and</strong>ard<br />
treatment with chloroquine eradicates the parasite.<br />
Following treatment <strong>of</strong> an acute attack <strong>of</strong> vivax malaria with<br />
schizonticides, or a period <strong>of</strong> protection with prophylactic<br />
drugs, febrile illness can recur. Such relapsing illness can be prevented<br />
(or treated) by eradicating the parasites in the liver with<br />
primaquine, as described above. Proguanil hydrochloride<br />
administered continuously for three years, in order to suppress<br />
the parasites <strong>and</strong> allow time for the hepatic stages to die out naturally,<br />
is a useful alternative for patients with G6PD deficiency.<br />
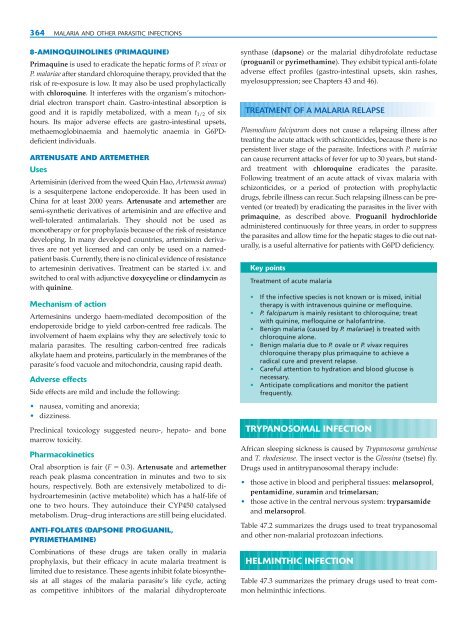
Key points<br />
Treatment <strong>of</strong> acute malaria<br />
• If the infective species is not known or is mixed, initial<br />
therapy is with intravenous quinine or mefloquine.<br />
• P. falciparum is mainly resistant to chloroquine; treat<br />
with quinine, mefloquine or hal<strong>of</strong>antrine.<br />
• Benign malaria (caused by P. malariae) is treated with<br />
chloroquine alone.<br />
• Benign malaria due to P. ovale or P. vivax requires<br />
chloroquine therapy plus primaquine to achieve a<br />
radical cure <strong>and</strong> prevent relapse.<br />
• Careful attention to hydration <strong>and</strong> blood glucose is<br />
necessary.<br />
• Anticipate complications <strong>and</strong> monitor the patient<br />
frequently.<br />
TRYPANOSOMAL INFECTION<br />
African sleeping sickness is caused by Trypanosoma gambiense<br />
<strong>and</strong> T. rhodesiense. The insect vector is the Glossina (tsetse) fly.<br />
Drugs used in antitrypanosomal therapy include:<br />
• those active in blood <strong>and</strong> peripheral tissues: melarsoprol,<br />
pentamidine, suramin <strong>and</strong> trimelarsan;<br />
• those active in the central nervous system: tryparsamide<br />
<strong>and</strong> melarsoprol.<br />
Table 47.2 summarizes the drugs used to treat trypanosomal<br />
<strong>and</strong> other non-malarial protozoan infections.<br />
HELMINTHIC INFECTION<br />
Table 47.3 summarizes the primary drugs used to treat common<br />
helminthic infections.