A-Textbook-of-Clinical-Pharmacology-and-Therapeutics-5th-edition
A-Textbook-of-Clinical-Pharmacology-and-Therapeutics-5th-edition
A-Textbook-of-Clinical-Pharmacology-and-Therapeutics-5th-edition
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
DRUGS FOR HEART FAILURE 215<br />
therapeutic plasma concentration can be obtained more rapidly<br />
by administering a loading dose (Chapter 3).<br />
Mechanism <strong>of</strong> action<br />
Digoxin inhibits Na /K adenosine triphosphatase (Na /K <br />
ATPase). This causes accumulation <strong>of</strong> intracellular Na <strong>and</strong><br />
increased intracellular [Ca 2 ] concentrations via reduced<br />
Na /Ca 2 exchange. The rise in availability <strong>of</strong> intracellular Ca 2<br />
accounts for the positive inotropic effect <strong>of</strong> digoxin. Excessive<br />
inhibition <strong>of</strong> Na /K ATPase causes numerous non-cardiac as<br />
well as cardiac (dysrhythmogenic) toxic effects. Ventricular<br />
slowing results from increased vagal activity on the AV node.<br />
Slowing <strong>of</strong> ventricular rate improves cardiac output in patients<br />
with atrial fibrillation by improving ventricular filling during<br />
diastole. <strong>Clinical</strong> progress is assessed by measuring heart rate (at<br />
the apex): apical rates <strong>of</strong> 70–80 per minute can be achieved at<br />
rest. Unfortunately, since vagal activity is suppressed during<br />
exercise (when heart rate is controlled by sympathetic activation),<br />
control <strong>of</strong> rate during exercise is not usually achievable.<br />
Pharmacokinetics<br />
Approximately 80% is excreted unchanged in the urine<br />
in patients with normal renal function with a half-life <strong>of</strong><br />
30–48 hours. It is eliminated mainly by glomerular filtration,<br />
although small amounts are secreted <strong>and</strong> reabsorbed. A small<br />
amount (5–10%) undergoes metabolism to inactive products or<br />
excretion via the bile <strong>and</strong> elimination in faeces. The proportion<br />
eliminated by these non-renal clearance mechanisms increases<br />
in patients with renal impairment, being 100% in anephric<br />
patients, in whom the half-life is approximately 4.5 days.<br />
Blood for digoxin concentration determination should be<br />
sampled more than six hours after an oral dose or immediately<br />
before the next dose is due (trough level) to allow its tissue<br />
distribution to be complete. The usual therapeutic range is<br />
1–2 ng/mL, although toxicity can occur at concentrations <strong>of</strong><br />
less than 1.5 ng/mL in some individuals.<br />
Drug interactions<br />
Digoxin has a steep dose–response curve <strong>and</strong> a narrow therapeutic<br />
range, <strong>and</strong> clinically important interactions are common<br />
(see Chapters 13 <strong>and</strong> 32). Pharmacokinetic interactions<br />
with digoxin include combined pharmacokinetic effects involving<br />
displacement from tissue-binding sites <strong>and</strong> reduced renal<br />
elimination (e.g. digoxin toxicity due to concurrent treatment<br />
with amiodarone or quinidine).<br />
Pharmacodynamic interactions are also important. In<br />
particular, drugs that cause hypokalaemia (e.g. diuretics,<br />
β-agonists, glucocorticoids) predispose to digoxin toxicity by<br />
increasing its binding to (<strong>and</strong> effect on) Na /K ATPase.<br />
OTHER POSITIVE INOTROPES<br />
Positive inotropes for intravenous infusion (e.g. adrenaline)<br />
have a place in treating acute shock, but not for chronic heart<br />
failure. Orally active positive inotropes other than digoxin<br />
include phosphodiesterase inhibitors, e.g. milrinone. These<br />
increase cardiac output <strong>and</strong> may bring some symptomatic<br />
benefit, but they worsen survival.<br />
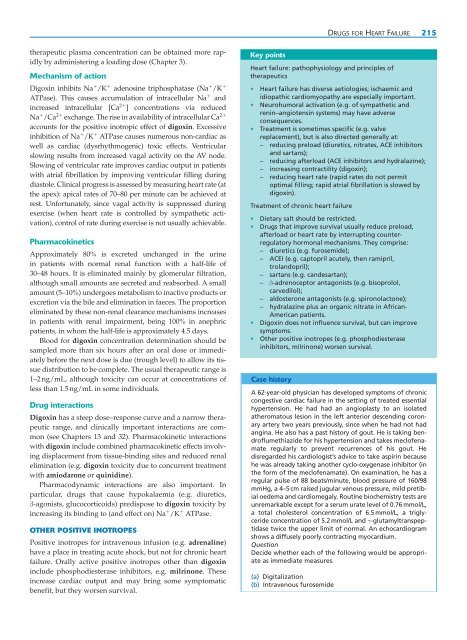
Key points<br />
Heart failure: pathophysiology <strong>and</strong> principles <strong>of</strong><br />
therapeutics<br />
• Heart failure has diverse aetiologies; ischaemic <strong>and</strong><br />
idiopathic cardiomyopathy are especially important.<br />
• Neurohumoral activation (e.g. <strong>of</strong> sympathetic <strong>and</strong><br />
renin–angiotensin systems) may have adverse<br />
consequences.<br />
• Treatment is sometimes specific (e.g. valve<br />
replacement), but is also directed generally at:<br />
– reducing preload (diuretics, nitrates, ACE inhibitors<br />
<strong>and</strong> sartans);<br />
– reducing afterload (ACE inhibitors <strong>and</strong> hydralazine);<br />
– increasing contractility (digoxin);<br />
– reducing heart rate (rapid rates do not permit<br />
optimal filling; rapid atrial fibrillation is slowed by<br />
digoxin).<br />
Treatment <strong>of</strong> chronic heart failure<br />
• Dietary salt should be restricted.<br />
• Drugs that improve survival usually reduce preload,<br />
afterload or heart rate by interrupting counterregulatory<br />
hormonal mechanisms. They comprise:<br />
– diuretics (e.g. furosemide);<br />
– ACEI (e.g. captopril acutely, then ramipril,<br />
trol<strong>and</strong>opril);<br />
– sartans (e.g. c<strong>and</strong>esartan);<br />
– β-adrenoceptor antagonists (e.g. bisoprolol,<br />
carvedilol);<br />
– aldosterone antagonists (e.g. spironolactone);<br />
– hydralazine plus an organic nitrate in African-<br />
American patients.<br />
• Digoxin does not influence survival, but can improve<br />
symptoms.<br />
• Other positive inotropes (e.g. phosphodiesterase<br />
inhibitors, milrinone) worsen survival.<br />
Case history<br />
A 62-year-old physician has developed symptoms <strong>of</strong> chronic<br />
congestive cardiac failure in the setting <strong>of</strong> treated essential<br />
hypertension. He had had an angioplasty to an isolated<br />
atheromatous lesion in the left anterior descending coronary<br />
artery two years previously, since when he had not had<br />
angina. He also has a past history <strong>of</strong> gout. He is taking bendr<strong>of</strong>lumethiazide<br />
for his hypertension <strong>and</strong> takes mecl<strong>of</strong>enamate<br />
regularly to prevent recurrences <strong>of</strong> his gout. He<br />
disregarded his cardiologist’s advice to take aspirin because<br />
he was already taking another cyclo-oxygenase inhibitor (in<br />
the form <strong>of</strong> the mecl<strong>of</strong>enamate). On examination, he has a<br />
regular pulse <strong>of</strong> 88 beats/minute, blood pressure <strong>of</strong> 160/98<br />
mmHg, a 4–5 cm raised jugular venous pressure, mild pretibial<br />
oedema <strong>and</strong> cardiomegaly. Routine biochemistry tests are<br />
unremarkable except for a serum urate level <strong>of</strong> 0.76 mmol/L,<br />
a total cholesterol concentration <strong>of</strong> 6.5 mmol/L, a triglyceride<br />
concentration <strong>of</strong> 5.2 mmol/L <strong>and</strong> γ-glutamyltranspeptidase<br />
twice the upper limit <strong>of</strong> normal. An echocardiogram<br />
shows a diffusely poorly contracting myocardium.<br />
Question<br />
Decide whether each <strong>of</strong> the following would be appropriate<br />
as immediate measures.<br />
(a) Digitalization<br />
(b) Intravenous furosemide