A-Textbook-of-Clinical-Pharmacology-and-Therapeutics-5th-edition
A-Textbook-of-Clinical-Pharmacology-and-Therapeutics-5th-edition
A-Textbook-of-Clinical-Pharmacology-and-Therapeutics-5th-edition
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
PEPTIC ULCERATION 249<br />
• With regard to drug therapy, several drugs (see below) are<br />
effective. Documented duodenal or gastric ulcerations<br />
should be treated with an H 2 -blocker or proton-pump<br />
inhibitor.<br />
• Test for the presence <strong>of</strong> H. pylori by using the urease CLO<br />
test or antral biopsy at endoscopy.<br />
• All suspected gastric ulcers should be endoscoped <strong>and</strong><br />
biopsied to exclude malignancy, with repeat endoscopy<br />
following treatment, to confirm healing <strong>and</strong> for repeat<br />
biopsy.<br />
• The current recommendation in relation to H. pylori is<br />
summarized above.<br />
Key points<br />
General management <strong>of</strong> peptic ulceration<br />
• Stop smoking.<br />
• Avoid ulcerogenic drugs (e.g. NSAIDs, alcohol,<br />
glucocorticosteroids).<br />
• Reduce caffeine intake.<br />
• Diet should be healthy (avoid obesity, <strong>and</strong> foods that<br />
give rise to symptoms).<br />
• Test for the presence <strong>of</strong> H. pylori.<br />
The choice <strong>of</strong> regimen used to eradicate H. pylori is<br />
based on achieving a balance between efficacy, adverse effects,<br />
compliance <strong>and</strong> cost. Most regimens include a combination<br />
<strong>of</strong> acid suppression <strong>and</strong> effective doses <strong>of</strong> two antibiotics.<br />
A typical regime for eradication <strong>of</strong> H. pylori is shown in<br />
Table 34.1.<br />
Eradication should be confirmed, preferably by urea breath<br />
test at a minimum <strong>of</strong> four weeks post-treatment.<br />
Non-steroidal anti-inflammatory<br />
drug-associated ulcer<br />
NSAID-related ulcers will usually heal if the NSAID is withdrawn<br />
<strong>and</strong> a proton-pump inhibitor is prescribed for four<br />
weeks. If the NSAID has to be restarted (preferably after healing),<br />
H 2 -receptor antagonists or proton-pump inhibitors or<br />
misoprostol (see below) should be co-prescribed. If H. pylori is<br />
present it should be eradicated.<br />
Key points<br />
Ulcer-healing drugs<br />
Reduction <strong>of</strong> acidity:<br />
• antacids;<br />
• H 2 -blockers;<br />
• proton-pump inhibitors;<br />
• muscarinic blockers (pirenzapine).<br />
Mucosal protection:<br />
• misoprostol (also reduces gastric acid secretion);<br />
• bismuth chelate (also toxic to H. pylori);<br />
• sucralfate;<br />
• carbenoxolone (rarely prescribed).<br />
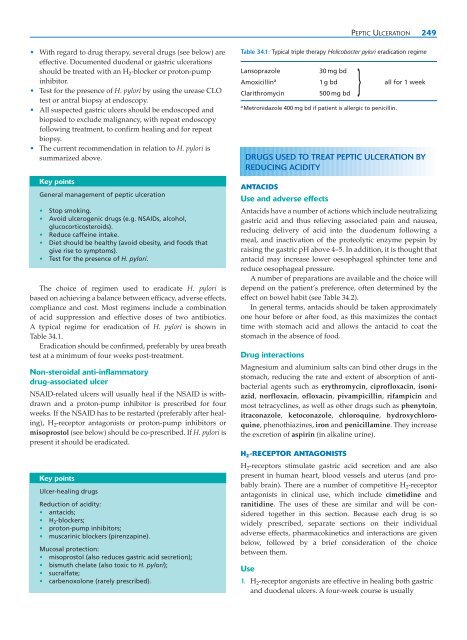
Table 34.1: Typical triple therapy Helicobacter pylori eradication regime<br />
Lansoprazole<br />
30 mg bd<br />
}<br />
Amoxicillin a 1 g bd all for 1 week<br />
Clarithromycin<br />
500 mg bd<br />
a Metronidazole 400 mg bd if patient is allergic to penicillin.<br />
DRUGS USED TO TREAT PEPTIC ULCERATION BY<br />
REDUCING ACIDITY<br />
ANTACIDS<br />
Use <strong>and</strong> adverse effects<br />
Antacids have a number <strong>of</strong> actions which include neutralizing<br />
gastric acid <strong>and</strong> thus relieving associated pain <strong>and</strong> nausea,<br />
reducing delivery <strong>of</strong> acid into the duodenum following a<br />
meal, <strong>and</strong> inactivation <strong>of</strong> the proteolytic enzyme pepsin by<br />
raising the gastric pH above 4–5. In addition, it is thought that<br />
antacid may increase lower oesophageal sphincter tone <strong>and</strong><br />
reduce oesophageal pressure.<br />
A number <strong>of</strong> preparations are available <strong>and</strong> the choice will<br />
depend on the patient’s preference, <strong>of</strong>ten determined by the<br />
effect on bowel habit (see Table 34.2).<br />
In general terms, antacids should be taken approximately<br />
one hour before or after food, as this maximizes the contact<br />
time with stomach acid <strong>and</strong> allows the antacid to coat the<br />
stomach in the absence <strong>of</strong> food.<br />
Drug interactions<br />
Magnesium <strong>and</strong> aluminium salts can bind other drugs in the<br />
stomach, reducing the rate <strong>and</strong> extent <strong>of</strong> absorption <strong>of</strong> antibacterial<br />
agents such as erythromycin, cipr<strong>of</strong>loxacin, isoniazid,<br />
norfloxacin, <strong>of</strong>loxacin, pivampicillin, rifampicin <strong>and</strong><br />
most tetracyclines, as well as other drugs such as phenytoin,<br />
itraconazole, ketoconazole, chloroquine, hydroxychloroquine,<br />
phenothiazines, iron <strong>and</strong> penicillamine. They increase<br />
the excretion <strong>of</strong> aspirin (in alkaline urine).<br />
H 2 -RECEPTOR ANTAGONISTS<br />
H 2 -receptors stimulate gastric acid secretion <strong>and</strong> are also<br />
present in human heart, blood vessels <strong>and</strong> uterus (<strong>and</strong> probably<br />
brain). There are a number <strong>of</strong> competitive H 2 -receptor<br />
antagonists in clinical use, which include cimetidine <strong>and</strong><br />
ranitidine. The uses <strong>of</strong> these are similar <strong>and</strong> will be considered<br />
together in this section. Because each drug is so<br />
widely prescribed, separate sections on their individual<br />
adverse effects, pharmacokinetics <strong>and</strong> interactions are given<br />
below, followed by a brief consideration <strong>of</strong> the choice<br />
between them.<br />
Use<br />
1. H 2 -receptor angonists are effective in healing both gastric<br />
<strong>and</strong> duodenal ulcers. A four-week course is usually