A-Textbook-of-Clinical-Pharmacology-and-Therapeutics-5th-edition
A-Textbook-of-Clinical-Pharmacology-and-Therapeutics-5th-edition
A-Textbook-of-Clinical-Pharmacology-and-Therapeutics-5th-edition
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
MANAGEMENT OF UNSTABLE CORONARY DISEASE 199<br />
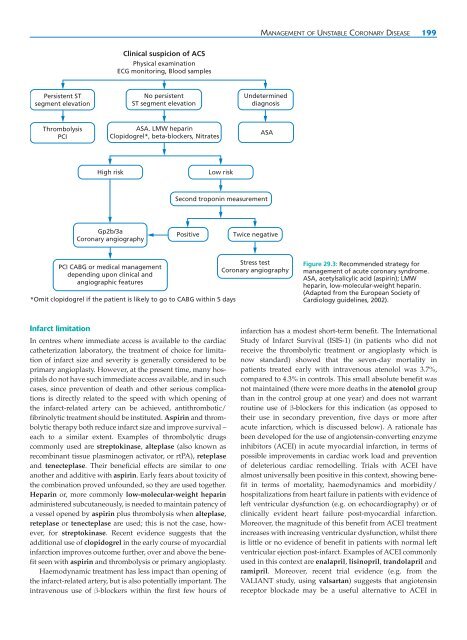
<strong>Clinical</strong> suspicion <strong>of</strong> ACS<br />
Physical examination<br />
ECG monitoring, Blood samples<br />
Persistent ST<br />
segment elevation<br />
No persistent<br />
ST segment elevation<br />
Undetermined<br />
diagnosis<br />
Thrombolysis<br />
PCI<br />
ASA. LMW heparin<br />
Clopidogrel*, beta-blockers, Nitrates<br />
ASA<br />
High risk<br />
Low risk<br />
Second troponin measurement<br />
Gp2b/3a<br />
Coronary angiography<br />
Positive<br />
Twice negative<br />
PCI CABG or medical management<br />
depending upon clinical <strong>and</strong><br />
angiographic features<br />
*Omit clopidogrel if the patient is likely to go to CABG within 5 days<br />
Stress test<br />
Coronary angiography<br />
Figure 29.3: Recommended strategy for<br />
management <strong>of</strong> acute coronary syndrome.<br />
ASA, acetylsalicylic acid (aspirin); LMW<br />
heparin, low-molecular-weight heparin.<br />
(Adapted from the European Society <strong>of</strong><br />
Cardiology guidelines, 2002).<br />
Infarct limitation<br />
In centres where immediate access is available to the cardiac<br />
catheterization laboratory, the treatment <strong>of</strong> choice for limitation<br />
<strong>of</strong> infarct size <strong>and</strong> severity is generally considered to be<br />
primary angioplasty. However, at the present time, many hospitals<br />
do not have such immediate access available, <strong>and</strong> in such<br />
cases, since prevention <strong>of</strong> death <strong>and</strong> other serious complications<br />
is directly related to the speed with which opening <strong>of</strong><br />
the infarct-related artery can be achieved, antithrombotic/<br />
fibrinolytic treatment should be instituted. Aspirin <strong>and</strong> thrombolytic<br />
therapy both reduce infarct size <strong>and</strong> improve survival –<br />
each to a similar extent. Examples <strong>of</strong> thrombolytic drugs<br />
commonly used are streptokinase, alteplase (also known as<br />
recombinant tissue plasminogen activator, or rtPA), reteplase<br />
<strong>and</strong> tenecteplase. Their beneficial effects are similar to one<br />
another <strong>and</strong> additive with aspirin. Early fears about toxicity <strong>of</strong><br />
the combination proved unfounded, so they are used together.<br />
Heparin or, more commonly low-molecular-weight heparin<br />
administered subcutaneously, is needed to maintain patency <strong>of</strong><br />
a vessel opened by aspirin plus thrombolysis when alteplase,<br />
reteplase or tenecteplase are used; this is not the case, however,<br />
for streptokinase. Recent evidence suggests that the<br />
additional use <strong>of</strong> clopidogrel in the early course <strong>of</strong> myocardial<br />
infarction improves outcome further, over <strong>and</strong> above the benefit<br />
seen with aspirin <strong>and</strong> thrombolysis or primary angioplasty.<br />
Haemodynamic treatment has less impact than opening <strong>of</strong><br />
the infarct-related artery, but is also potentially important. The<br />
intravenous use <strong>of</strong> β-blockers within the first few hours <strong>of</strong><br />
infarction has a modest short-term benefit. The International<br />
Study <strong>of</strong> Infarct Survival (ISIS-1) (in patients who did not<br />
receive the thrombolytic treatment or angioplasty which is<br />
now st<strong>and</strong>ard) showed that the seven-day mortality in<br />
patients treated early with intravenous atenolol was 3.7%,<br />
compared to 4.3% in controls. This small absolute benefit was<br />
not maintained (there were more deaths in the atenolol group<br />
than in the control group at one year) <strong>and</strong> does not warrant<br />
routine use <strong>of</strong> β-blockers for this indication (as opposed to<br />
their use in secondary prevention, five days or more after<br />
acute infarction, which is discussed below). A rationale has<br />
been developed for the use <strong>of</strong> angiotensin-converting enzyme<br />
inhibitors (ACEI) in acute myocardial infarction, in terms <strong>of</strong><br />
possible improvements in cardiac work load <strong>and</strong> prevention<br />
<strong>of</strong> deleterious cardiac remodelling. Trials with ACEI have<br />
almost universally been positive in this context, showing benefit<br />
in terms <strong>of</strong> mortality, haemodynamics <strong>and</strong> morbidity/<br />
hospitalizations from heart failure in patients with evidence <strong>of</strong><br />
left ventricular dysfunction (e.g. on echocardiography) or <strong>of</strong><br />
clinically evident heart failure post-myocardial infarction.<br />
Moreover, the magnitude <strong>of</strong> this benefit from ACEI treatment<br />
increases with increasing ventricular dysfunction, whilst there<br />
is little or no evidence <strong>of</strong> benefit in patients with normal left<br />
ventricular ejection post-infarct. Examples <strong>of</strong> ACEI commonly<br />
used in this context are enalapril, lisinopril, tr<strong>and</strong>olapril <strong>and</strong><br />
ramipril. Moreover, recent trial evidence (e.g. from the<br />
VALIANT study, using valsartan) suggests that angiotensin<br />
receptor blockade may be a useful alternative to ACEI in