June 2017
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
SENIORS<br />
Let’s Talk About<br />
Death and Dying<br />
by Rose Tucker MSN, RN<br />
Death and the dying process is probably the last topic<br />
anyone wishes to discuss. But whether we like it or<br />
not, we may be asked to make end-of-life decisions<br />
for our loved ones without knowing their preferences.<br />
It can be both emotionally draining on family to make these<br />
choices and confusing as physicians and health-care<br />
professionals use medical terms we may not fully understand.<br />
As a registered nurse for nearly 30 years, I have had the<br />
privilege to care for many people at the end-of-life and offer<br />
support and guidance to their family members. The following<br />
is some advice I have for anyone asked to make such difficult<br />
decisions for a loved one admitted to the hospital and I also<br />
discuss some common misconceptions about end-of-life care.<br />
Our bodies are so complex and weaken differently that each<br />
situation is approached differently. But one general question<br />
that will need to be addressed in all end-of-life situations is<br />
code status. When a person is admitted to the hospital they<br />
will be asked if they have a “living will.” This is a document<br />
that the patient may have signed prior to their decline in health<br />
that indicates they do not wish to be kept alive artificially if<br />
their condition is terminal. Unfortunately, not many of us have<br />
prepared a living will in advance and now these decisions are<br />
left to a spouse or close relative, or some other adult who has<br />
been designated to act as the patient’s health care surrogate.<br />
The options for<br />
code status are ‘full<br />
code’ or ‘do not<br />
resuscitate’ (DNR).<br />
A full code means<br />
that as respirations<br />
and heart function<br />
become impaired<br />
and will soon stop,<br />
cardiopulmonary<br />
resuscitation is<br />
performed. CPR consists of compressing the patient’s chest<br />
two inches at a rate of 100 times per minute until the patient is<br />
either revived or the heart is unable to be restarted and death<br />
ensues. If resuscitation is resumed, the patient will be on what<br />
is often called ‘life-support.’ This means that the patient will now<br />
be on a ventilator that will be breathing for them. The patient will<br />
then be transferred to a critical care area of the hospital if not<br />
already there.<br />
96<br />
JUNE <strong>2017</strong><br />
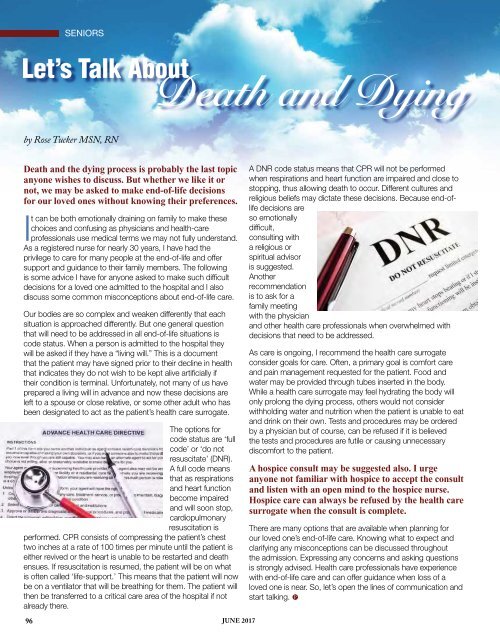
A DNR code status means that CPR will not be performed<br />
when respirations and heart function are impaired and close to<br />
stopping, thus allowing death to occur. Different cultures and<br />
religious beliefs may dictate these decisions. Because end-oflife<br />
decisions are<br />
so emotionally<br />
difficult,<br />
consulting with<br />
a religious or<br />
spiritual advisor<br />
is suggested.<br />
Another<br />
recommendation<br />
is to ask for a<br />
family meeting<br />
with the physician<br />
and other health care professionals when overwhelmed with<br />
decisions that need to be addressed.<br />
As care is ongoing, I recommend the health care surrogate<br />
consider goals for care. Often, a primary goal is comfort care<br />
and pain management requested for the patient. Food and<br />
water may be provided through tubes inserted in the body.<br />
While a health care surrogate may feel hydrating the body will<br />
only prolong the dying process, others would not consider<br />
withholding water and nutrition when the patient is unable to eat<br />
and drink on their own. Tests and procedures may be ordered<br />
by a physician but of course, can be refused if it is believed<br />
the tests and procedures are futile or causing unnecessary<br />
discomfort to the patient.<br />
A hospice consult may be suggested also. I urge<br />
anyone not familiar with hospice to accept the consult<br />
and listen with an open mind to the hospice nurse.<br />
Hospice care can always be refused by the health care<br />
surrogate when the consult is complete.<br />
There are many options that are available when planning for<br />
our loved one’s end-of-life care. Knowing what to expect and<br />
clarifying any misconceptions can be discussed throughout<br />
the admission. Expressing any concerns and asking questions<br />
is strongly advised. Health care professionals have experience<br />
with end-of-life care and can offer guidance when loss of a<br />
loved one is near. So, let’s open the lines of communication and<br />
start talking. P