Richtlijn Sterilisatie van de vrouw - NVOG
Richtlijn Sterilisatie van de vrouw - NVOG
Richtlijn Sterilisatie van de vrouw - NVOG
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
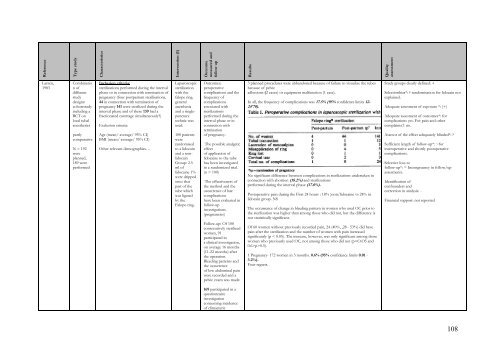
ReferenceType studyCharacteristicsIntervention (I)Outcomemeasured andfollow upResultsQualityassessmentLarsen,1983Combination ofdifferentstudy<strong>de</strong>signs:cohortstudyincluding aRCT onlocal tubalanestheticspartlycomparativeN = 192wereplanned,189 wereperformedInclusion criteria:sterilizations performed during the intervalphase or in connection with termination ofpregnancy (four postpartum sterilisations,44 in connection with termination ofpregnancy 141 were sterilized during theinterval phase and of these 139 had afractionated curettage simultaneously?)Exclusion criteria:Age (mean/ average/ 95% CI)BMI (mean/ average/ 95% CI)Other rele<strong>van</strong>t <strong>de</strong>mographics…Laparoscopicsterilizationwith thefalope ring.generalanesthesiaand a singlepuncturetechnic wasused.100 patientswererandomisedto a lidocainand a nonlidocainGroup: 2.5ml oflidocaine 1%were drippedonto thatpart of thetube whichwas ligatedby theFalope-ring.Outcomes:peroperativecomplications and thefrequency ofcomplicationsassociated withsterilizationsperformed during theinterval phase or inconnection withterminationof pregnancy.The possible analgeticeffectof application oflidocaine to the tubehas been investigatedin a randomized trial.(n = 100)The effectiveness ofthe method and theoccurrence of latecomplicationshave been evaluated infollow-upinvestigations.(pregnancies)Follow-up: Of 100consecutively sterilizedwomen, 91participated ina clinical investigation,on average 16 months(11-22 months) afterthe operation.Bleeding patterns andthe occurrenceof low abdominal painwere recor<strong>de</strong>d and apelvic exam was ma<strong>de</strong>.3 planned procedures were abbandoned because of failure to visualize the tubesbecause of pelvicadhesions (2 cases) or equipment malfunction (1 case).In all, the frequency of complications was 17.5% (95% confi<strong>de</strong>nce limits 12-24'70).No significant difference between complications in sterilizations un<strong>de</strong>rtaken inconnection with abortion (18.2%) and sterilizationsperformed during the interval phase (17.0%).Postoperative pain during the First 24 hours : 18% )non/lidocaine vs 24% inlidocain group. NSThe occurrence of change in bleeding pattern in women who used OC prior tothe sterilization was higher than among those who did not, but the difference isnot statistically significant.Of 60 women without previously recor<strong>de</strong>d pain, 24 (40%, ,28 - 53%) did havepain after the sterilization and the number of women with pain increasedsignificantly (p < 0.05). The increase, however, was only significant among thosewomen who previously used OC, not among those who did not (pp>0.5).1 Pregnancy- 172 women in 3 months. 0.6% (95% confi<strong>de</strong>nce limits 0.01 -3.2%).Four regrets.Study groups clearly <strong>de</strong>fined: +Selectionbias*: ? randomisation for lidocain notexplained.A<strong>de</strong>quate assesment of exposure *: (+)A<strong>de</strong>quate assesment of outcomes*: forcomplications yes. For pain and othercomplaints± no.Assesor of the effect a<strong>de</strong>quately blin<strong>de</strong>d*: ?Sufficient length of follow-up*: ~forinteroperative and shortly postoperativecomplications.Selective loss tofollow-up*: = Incongruency in follow/upassesments.I<strong>de</strong>ntification ofconfoun<strong>de</strong>rs andcorrection in analysis: -Financial support: not reported169 participated in aquestionnaireinvestigationconcerning inci<strong>de</strong>nceof climacteric108