A Guide to Primary Care of People with HIV/AIDS - Canadian Public ...
A Guide to Primary Care of People with HIV/AIDS - Canadian Public ...
A Guide to Primary Care of People with HIV/AIDS - Canadian Public ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
A <strong>Guide</strong> <strong>to</strong> <strong>Primary</strong> <strong>Care</strong> <strong>of</strong> <strong>People</strong> <strong>with</strong> <strong>HIV</strong>/<strong>AIDS</strong><br />
Chapter 15: Palliative and End-<strong>of</strong>-Life <strong>Care</strong><br />
• Reduction <strong>of</strong> diagnostic studies and number <strong>of</strong><br />
medications as prognosis shortens<br />
• Regular review <strong>of</strong> health power <strong>of</strong> at<strong>to</strong>rney and<br />
support <strong>of</strong> patient wishes<br />
• Discussions <strong>of</strong> prognosis <strong>with</strong> patient and family soon<br />
enough <strong>to</strong> allow closure near the end <strong>of</strong> life<br />
• Referral <strong>to</strong> hospice/palliative home care when <strong>of</strong>fice<br />
visits become burdensome for patient<br />
• Maintenance <strong>of</strong> contact <strong>with</strong> family during<br />
bereavement period<br />
• Acknowledgement <strong>of</strong> staff members’ feelings <strong>of</strong> loss<br />
when patients die<br />
What are some common symp<strong>to</strong>ms experienced<br />
by persons <strong>with</strong> advanced <strong>HIV</strong> disease?<br />
In surveys, patients receiving ART report experiencing<br />
the same symp<strong>to</strong>ms as patients reported in the earlier<br />
years <strong>of</strong> the epidemic, but the frequencies <strong>of</strong> symp<strong>to</strong>ms<br />
have changed (Mathews et al, 2000; Vogl et al, 1998).<br />
Fatigue, sadness, diarrhea, and fever continue <strong>to</strong> plague<br />
patients even when disease is controlled by ART. Pain<br />
is still experienced by up <strong>to</strong> 75% <strong>of</strong> patients and may<br />
be present in multiple areas at once, including the<br />
extremities and oral, esophageal, abdominal, or rectal<br />
sites. Adequate treatment for one type <strong>of</strong> pain may<br />
only expose another. This <strong>of</strong>ten raises the specter <strong>of</strong><br />
“drug-seeking behavior” when in fact the patient is<br />
simply able <strong>to</strong> be aware <strong>of</strong> the secondary pain after the<br />
greater pain is relieved (see Chapter 13, Management <strong>of</strong><br />
Substance Abuse). Peripheral neuropathy can be caused<br />
by ART, <strong>HIV</strong> disease itself, or unrelated disease such as<br />
diabetes. This pain does not seem <strong>to</strong> be related <strong>to</strong> the<br />
degree <strong>of</strong> control <strong>of</strong> viral burden, and cause must be<br />
sought through his<strong>to</strong>rytaking as many patients seem<br />
<strong>to</strong> overlook early manifestations such as numbness.<br />
Refer <strong>to</strong> Chapter 8, Symp<strong>to</strong>m Management, as well as<br />
resources under Suggested Resources for management<br />
<strong>of</strong> pain and symp<strong>to</strong>ms.<br />
How important is pain control in advanced<br />
<strong>HIV</strong> disease?<br />
Pain, as <strong>with</strong> any symp<strong>to</strong>m, should be described,<br />
quantitated, treated, and promptly reevaluated <strong>with</strong><br />
appropriate dose modification <strong>of</strong> therapy (see Table 15-1).<br />
In the <strong>Guide</strong>lines for Management <strong>of</strong> Cancer Pain, pain<br />
experienced by those <strong>with</strong> <strong>HIV</strong> disease is compared<br />
<strong>with</strong> the chronic pain experienced by persons <strong>with</strong><br />
cancer, which <strong>of</strong>ten requires management <strong>with</strong> opioids<br />
(AHCPR, 1994). Unlike blood pressure, which might be<br />
regulated over weeks, pain should be controlled <strong>with</strong>in<br />
the shortest time possible <strong>to</strong> prevent the development<br />
<strong>of</strong> long-term symp<strong>to</strong>ms such as depression and<br />
anhedonia.<br />
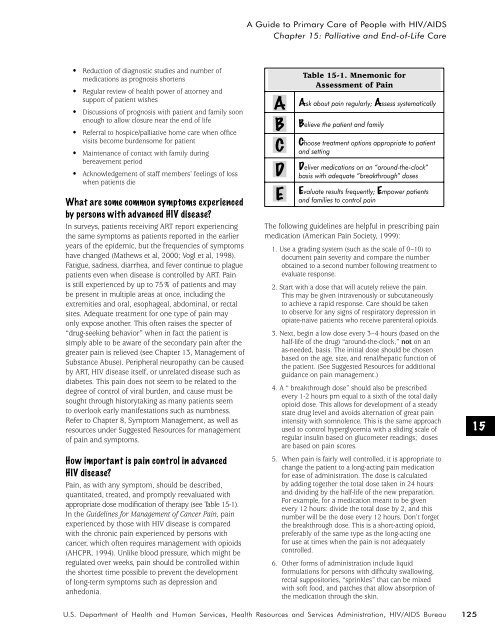
A<br />
B<br />
C<br />
D<br />
E<br />
Table 15-1. Mnemonic for<br />
Assessment <strong>of</strong> Pain<br />
Ask about pain regularly; Assess systematically<br />
Believe the patient and family<br />
Choose treatment options appropriate <strong>to</strong> patient<br />
and setting<br />
Deliver medications on an “around-the-clock”<br />
basis <strong>with</strong> adequate “breakthrough” doses<br />
Evaluate results frequently; Empower patients<br />
and families <strong>to</strong> control pain<br />
The following guidelines are helpful in prescribing pain<br />
medication (American Pain Society, 1999):<br />
1. Use a grading system (such as the scale <strong>of</strong> 0–10) <strong>to</strong><br />
document pain severity and compare the number<br />
obtained <strong>to</strong> a second number following treatment <strong>to</strong><br />
evaluate response.<br />
2. Start <strong>with</strong> a dose that will acutely relieve the pain.<br />
This may be given intravenously or subcutaneously<br />
<strong>to</strong> achieve a rapid response. <strong>Care</strong> should be taken<br />
<strong>to</strong> observe for any signs <strong>of</strong> respira<strong>to</strong>ry depression in<br />
opiate-naive patients who receive parenteral opioids.<br />
3. Next, begin a low dose every 3–4 hours (based on the<br />
half-life <strong>of</strong> the drug) “around-the-clock,” not on an<br />
as-needed, basis. The initial dose should be chosen<br />
based on the age, size, and renal/hepatic function <strong>of</strong><br />
the patient. (See Suggested Resources for additional<br />
guidance on pain management.)<br />
4. A “ breakthrough dose” should also be prescribed<br />
every 1-2 hours prn equal <strong>to</strong> a sixth <strong>of</strong> the <strong>to</strong>tal daily<br />
opioid dose. This allows for development <strong>of</strong> a steady<br />
state drug level and avoids alternation <strong>of</strong> great pain<br />
intensity <strong>with</strong> somnolence. This is the same approach<br />
used <strong>to</strong> control hyperglycemia <strong>with</strong> a sliding scale <strong>of</strong><br />
regular insulin based on glucometer readings; doses<br />
are based on pain scores.<br />
5. When pain is fairly well controlled, it is appropriate <strong>to</strong><br />
change the patient <strong>to</strong> a long-acting pain medication<br />
for ease <strong>of</strong> administration. The dose is calculated<br />
by adding <strong>to</strong>gether the <strong>to</strong>tal dose taken in 24 hours<br />
and dividing by the half-life <strong>of</strong> the new preparation.<br />
For example, for a medication meant <strong>to</strong> be given<br />
every 12 hours: divide the <strong>to</strong>tal dose by 2, and this<br />
number will be the dose every 12 hours. Don’t forget<br />
the breakthrough dose. This is a short-acting opioid,<br />
preferably <strong>of</strong> the same type as the long-acting one<br />
for use at times when the pain is not adequately<br />
controlled.<br />
6. Other forms <strong>of</strong> administration include liquid<br />
formulations for persons <strong>with</strong> difficulty swallowing,<br />
rectal supposi<strong>to</strong>ries, “sprinkles” that can be mixed<br />
<strong>with</strong> s<strong>of</strong>t food, and patches that allow absorption <strong>of</strong><br />
the medication through the skin.<br />
15<br />
U.S. Department <strong>of</strong> Health and Human Services, Health Resources and Services Administration, <strong>HIV</strong>/<strong>AIDS</strong> Bureau<br />
125