A Guide to Primary Care of People with HIV/AIDS - Canadian Public ...
A Guide to Primary Care of People with HIV/AIDS - Canadian Public ...
A Guide to Primary Care of People with HIV/AIDS - Canadian Public ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
A <strong>Guide</strong> <strong>to</strong> <strong>Primary</strong> <strong>Care</strong> <strong>of</strong> <strong>People</strong> <strong>with</strong> <strong>HIV</strong>/<strong>AIDS</strong><br />
Chapter 2: Approach <strong>to</strong> the Patient<br />
2<br />
RISK ASSESSMENT AND<br />
COUNSELING<br />
What risk-taking behaviors should be reviewed<br />
<strong>with</strong> patients?<br />
Patients infected <strong>with</strong> <strong>HIV</strong> who practice unsafe sex or<br />
inject drugs can infect others, be reinfected themselves<br />
<strong>with</strong> new <strong>HIV</strong> strains, or contract STDs, viral hepatitis,<br />
or other infections. Abuse <strong>of</strong> alcohol or illicit drugs<br />
is directly harmful and may affect adherence <strong>to</strong> a<br />
complicated medical regimen. Accordingly, providers<br />
need a detailed understanding <strong>of</strong> their patients’<br />
risk-taking behaviors <strong>to</strong> guide patient education and<br />
counseling efforts and <strong>to</strong> assess the advisability <strong>of</strong><br />
initiating antiretroviral treatment.<br />
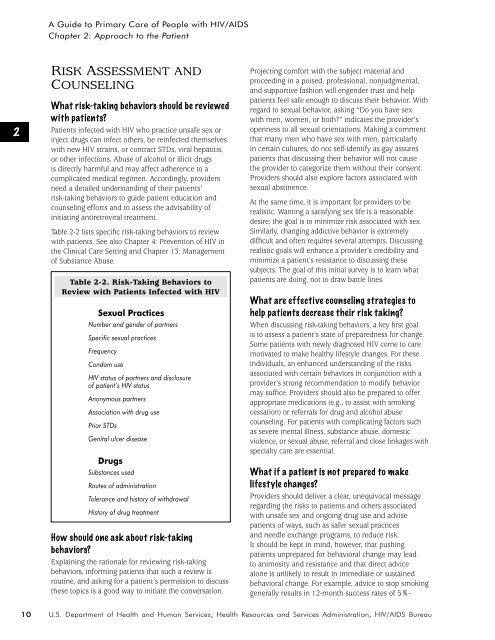
Table 2-2 lists specific risk-taking behaviors <strong>to</strong> review<br />
<strong>with</strong> patients. See also Chapter 4: Prevention <strong>of</strong> <strong>HIV</strong> in<br />
the Clinical <strong>Care</strong> Setting and Chapter 13: Management<br />
<strong>of</strong> Substance Abuse.<br />
Table 2-2. Risk-Taking Behaviors <strong>to</strong><br />
Review <strong>with</strong> Patients Infected <strong>with</strong> <strong>HIV</strong><br />
Sexual Practices<br />
Number and gender <strong>of</strong> partners<br />
Specific sexual practices<br />
Frequency<br />
Condom use<br />
<strong>HIV</strong> status <strong>of</strong> partners and disclosure<br />
<strong>of</strong> patient’s <strong>HIV</strong> status<br />
Anonymous partners<br />
Association <strong>with</strong> drug use<br />
Prior STDs<br />
Genital ulcer disease<br />
Drugs<br />
Substances used<br />
Routes <strong>of</strong> administration<br />
Tolerance and his<strong>to</strong>ry <strong>of</strong> <strong>with</strong>drawal<br />
His<strong>to</strong>ry <strong>of</strong> drug treatment<br />
How should one ask about risk-taking<br />
behaviors?<br />
Explaining the rationale for reviewing risk-taking<br />
behaviors, informing patients that such a review is<br />
routine, and asking for a patient’s permission <strong>to</strong> discuss<br />
these <strong>to</strong>pics is a good way <strong>to</strong> initiate the conversation.<br />
Projecting comfort <strong>with</strong> the subject material and<br />
proceeding in a poised, pr<strong>of</strong>essional, nonjudgmental,<br />
and supportive fashion will engender trust and help<br />
patients feel safe enough <strong>to</strong> discuss their behavior. With<br />
regard <strong>to</strong> sexual behavior, asking “Do you have sex<br />
<strong>with</strong> men, women, or both?” indicates the provider’s<br />
openness <strong>to</strong> all sexual orientations. Making a comment<br />
that many men who have sex <strong>with</strong> men, particularly<br />
in certain cultures, do not self-identify as gay assures<br />
patients that discussing their behavior will not cause<br />
the provider <strong>to</strong> categorize them <strong>with</strong>out their consent.<br />
Providers should also explore fac<strong>to</strong>rs associated <strong>with</strong><br />
sexual abstinence.<br />
At the same time, it is important for providers <strong>to</strong> be<br />
realistic. Wanting a satisfying sex life is a reasonable<br />
desire; the goal is <strong>to</strong> minimize risk associated <strong>with</strong> sex.<br />
Similarly, changing addictive behavior is extremely<br />
difficult and <strong>of</strong>ten requires several attempts. Discussing<br />
realistic goals will enhance a provider’s credibility and<br />
minimize a patient’s resistance <strong>to</strong> discussing these<br />
subjects. The goal <strong>of</strong> this initial survey is <strong>to</strong> learn what<br />
patients are doing, not <strong>to</strong> draw battle lines.<br />
What are effective counseling strategies <strong>to</strong><br />
help patients decrease their risk taking?<br />
When discussing risk-taking behaviors, a key first goal<br />
is <strong>to</strong> assess a patient’s state <strong>of</strong> preparedness for change.<br />
Some patients <strong>with</strong> newly diagnosed <strong>HIV</strong> come <strong>to</strong> care<br />
motivated <strong>to</strong> make healthy lifestyle changes. For these<br />
individuals, an enhanced understanding <strong>of</strong> the risks<br />
associated <strong>with</strong> certain behaviors in conjunction <strong>with</strong> a<br />
provider’s strong recommendation <strong>to</strong> modify behavior<br />
may suffice. Providers should also be prepared <strong>to</strong> <strong>of</strong>fer<br />
appropriate medications (e.g., <strong>to</strong> assist <strong>with</strong> smoking<br />
cessation) or referrals for drug and alcohol abuse<br />
counseling. For patients <strong>with</strong> complicating fac<strong>to</strong>rs such<br />
as severe mental illness, substance abuse, domestic<br />
violence, or sexual abuse, referral and close linkages <strong>with</strong><br />
specialty care are essential.<br />
What if a patient is not prepared <strong>to</strong> make<br />
lifestyle changes?<br />
Providers should deliver a clear, unequivocal message<br />
regarding the risks <strong>to</strong> patients and others associated<br />
<strong>with</strong> unsafe sex and ongoing drug use and advise<br />
patients <strong>of</strong> ways, such as safer sexual practices<br />
and needle exchange programs, <strong>to</strong> reduce risk.<br />
It should be kept in mind, however, that pushing<br />
patients unprepared for behavioral change may lead<br />
<strong>to</strong> animosity and resistance and that direct advice<br />
alone is unlikely <strong>to</strong> result in immediate or sustained<br />
behavioral change. For example, advice <strong>to</strong> s<strong>to</strong>p smoking<br />
generally results in 12-month success rates <strong>of</strong> 5%-<br />
10<br />
U.S. Department <strong>of</strong> Health and Human Services, Health Resources and Services Administration, <strong>HIV</strong>/<strong>AIDS</strong> Bureau