A Guide to Primary Care of People with HIV/AIDS - Canadian Public ...
A Guide to Primary Care of People with HIV/AIDS - Canadian Public ...
A Guide to Primary Care of People with HIV/AIDS - Canadian Public ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
A <strong>Guide</strong> <strong>to</strong> <strong>Primary</strong> <strong>Care</strong> <strong>of</strong> <strong>People</strong> <strong>with</strong> <strong>HIV</strong>/<strong>AIDS</strong><br />
Chapter 5: Antiretroviral Therapy<br />
5<br />
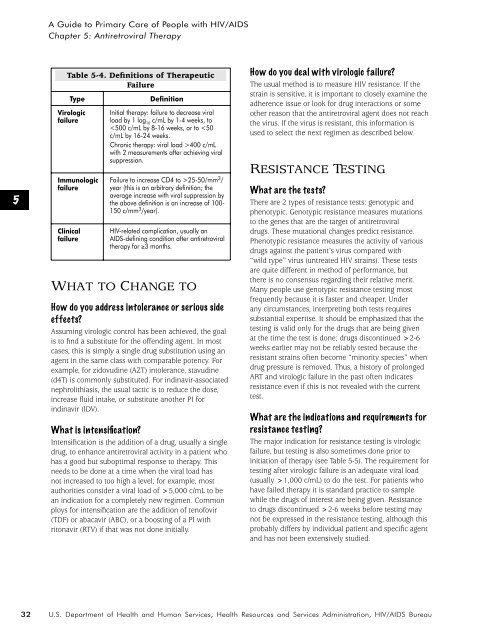
Table 5-4. Definitions <strong>of</strong> Therapeutic<br />
Failure<br />
Type<br />
Virologic<br />
failure<br />
Immunologic<br />
failure<br />
Clinical<br />
failure<br />
Definition<br />
Initial therapy: failure <strong>to</strong> decrease viral<br />
load by 1 log 10<br />
c/mL by 1-4 weeks, <strong>to</strong><br />
25-50/mm 3 /<br />
year (this is an arbitrary definition; the<br />
average increase <strong>with</strong> viral suppression by<br />
the above definition is an increase <strong>of</strong> 100-<br />
150 c/mm 3 /year).<br />
<strong>HIV</strong>-related complication, usually an<br />
<strong>AIDS</strong>-defining condition after antiretroviral<br />
therapy for ≥3 months.<br />
WHAT TO CHANGE TO<br />
How do you address in<strong>to</strong>lerance or serious side<br />
effects?<br />
Assuming virologic control has been achieved, the goal<br />
is <strong>to</strong> find a substitute for the <strong>of</strong>fending agent. In most<br />
cases, this is simply a single drug substitution using an<br />
agent in the same class <strong>with</strong> comparable potency. For<br />
example, for zidovudine (AZT) in<strong>to</strong>lerance, stavudine<br />
(d4T) is commonly substituted. For indinavir-associated<br />
nephrolithiasis, the usual tactic is <strong>to</strong> reduce the dose,<br />
increase fluid intake, or substitute another PI for<br />
indinavir (IDV).<br />
What is intensification?<br />
Intensification is the addition <strong>of</strong> a drug, usually a single<br />
drug, <strong>to</strong> enhance antiretroviral activity in a patient who<br />
has a good but suboptimal response <strong>to</strong> therapy. This<br />
needs <strong>to</strong> be done at a time when the viral load has<br />
not increased <strong>to</strong> <strong>to</strong>o high a level; for example, most<br />
authorities consider a viral load <strong>of</strong> >5,000 c/mL <strong>to</strong> be<br />
an indication for a completely new regimen. Common<br />
ploys for intensification are the addition <strong>of</strong> ten<strong>of</strong>ovir<br />
(TDF) or abacavir (ABC), or a boosting <strong>of</strong> a PI <strong>with</strong><br />
ri<strong>to</strong>navir (RTV) if that was not done initially.<br />
How do you deal <strong>with</strong> virologic failure?<br />
The usual method is <strong>to</strong> measure <strong>HIV</strong> resistance. If the<br />
strain is sensitive, it is important <strong>to</strong> closely examine the<br />
adherence issue or look for drug interactions or some<br />
other reason that the antiretroviral agent does not reach<br />
the virus. If the virus is resistant, this information is<br />
used <strong>to</strong> select the next regimen as described below.<br />
RESISTANCE TESTING<br />
What are the tests?<br />
There are 2 types <strong>of</strong> resistance tests: genotypic and<br />
phenotypic. Genotypic resistance measures mutations<br />
<strong>to</strong> the genes that are the target <strong>of</strong> antiretroviral<br />
drugs. These mutational changes predict resistance.<br />
Phenotypic resistance measures the activity <strong>of</strong> various<br />
drugs against the patient’s virus compared <strong>with</strong><br />
“wild type” virus (untreated <strong>HIV</strong> strains). These tests<br />
are quite different in method <strong>of</strong> performance, but<br />
there is no consensus regarding their relative merit.<br />
Many people use genotypic resistance testing most<br />
frequently because it is faster and cheaper. Under<br />
any circumstances, interpreting both tests requires<br />
substantial expertise. It should be emphasized that the<br />
testing is valid only for the drugs that are being given<br />
at the time the test is done; drugs discontinued >2-6<br />
weeks earlier may not be reliably tested because the<br />
resistant strains <strong>of</strong>ten become “minority species” when<br />
drug pressure is removed. Thus, a his<strong>to</strong>ry <strong>of</strong> prolonged<br />
ART and virologic failure in the past <strong>of</strong>ten indicates<br />
resistance even if this is not revealed <strong>with</strong> the current<br />
test.<br />
What are the indications and requirements for<br />
resistance testing?<br />
The major indication for resistance testing is virologic<br />
failure, but testing is also sometimes done prior <strong>to</strong><br />
initiation <strong>of</strong> therapy (see Table 5-5). The requirement for<br />
testing after virologic failure is an adequate viral load<br />
(usually >1,000 c/mL) <strong>to</strong> do the test. For patients who<br />
have failed therapy it is standard practice <strong>to</strong> sample<br />
while the drugs <strong>of</strong> interest are being given. Resistance<br />
<strong>to</strong> drugs discontinued >2-6 weeks before testing may<br />
not be expressed in the resistance testing, although this<br />
probably differs by individual patient and specific agent<br />
and has not been extensively studied.<br />
32<br />
U.S. Department <strong>of</strong> Health and Human Services, Health Resources and Services Administration, <strong>HIV</strong>/<strong>AIDS</strong> Bureau