A Guide to Primary Care of People with HIV/AIDS - Canadian Public ...
A Guide to Primary Care of People with HIV/AIDS - Canadian Public ...
A Guide to Primary Care of People with HIV/AIDS - Canadian Public ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
A <strong>Guide</strong> <strong>to</strong> <strong>Primary</strong> <strong>Care</strong> <strong>of</strong> <strong>People</strong> <strong>with</strong> <strong>HIV</strong>/<strong>AIDS</strong><br />
Chapter 4: Prevention <strong>of</strong> <strong>HIV</strong> in the Clinical <strong>Care</strong> Setting<br />
4<br />
for enhanced counseling. More frequent screening<br />
for STDs is appropriate <strong>with</strong> evidence or suspicion <strong>of</strong><br />
high-risk sexual behavior (eg, sex <strong>with</strong> a new partner,<br />
sexual activity <strong>with</strong>out consistent and correct condom<br />
use); however, there are no data <strong>to</strong> guide the precise<br />
frequency. More frequent screening might also be<br />
appropriate in asymp<strong>to</strong>matic men who have sex <strong>with</strong><br />
men (MSM) and younger women because <strong>of</strong> a higher<br />
STD prevalence among these demographic groups.<br />
The local prevalence <strong>of</strong> these infections might guide<br />
frequency <strong>of</strong> screening. Labora<strong>to</strong>ry screening for drug<br />
abuse is addressed in Chapter 13.<br />
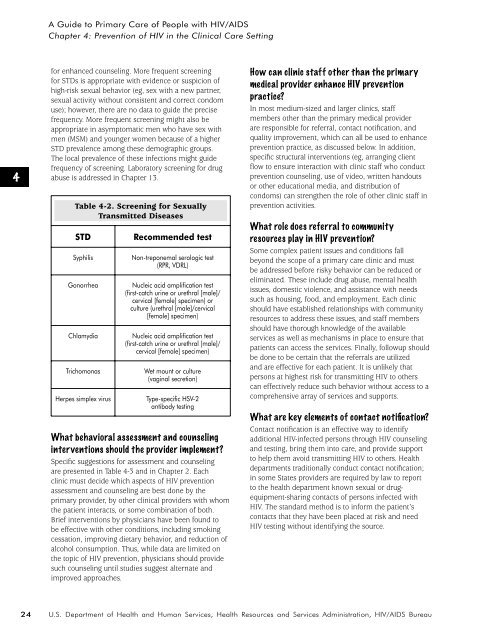
Table 4-2. Screening for Sexually<br />
Transmitted Diseases<br />
STD<br />
Syphilis<br />
Gonorrhea<br />
Chlamydia<br />
Trichomonas<br />
Herpes simplex virus<br />
Recommended test<br />
Non-treponemal serologic test<br />
(RPR, VDRL)<br />
Nucleic acid amplification test<br />
(first-catch urine or urethral [male]/<br />
cervical [female] specimen) or<br />
culture (urethral [male]/cervical<br />
[female] specimen)<br />
Nucleic acid amplification test<br />
(first-catch urine or urethral [male]/<br />
cervical [female] specimen)<br />
Wet mount or culture<br />
(vaginal secretion)<br />
Type-specific HSV-2<br />
antibody testing<br />
What behavioral assessment and counseling<br />
interventions should the provider implement?<br />
Specific suggestions for assessment and counseling<br />
are presented in Table 4-3 and in Chapter 2. Each<br />
clinic must decide which aspects <strong>of</strong> <strong>HIV</strong> prevention<br />
assessment and counseling are best done by the<br />
primary provider, by other clinical providers <strong>with</strong> whom<br />
the patient interacts, or some combination <strong>of</strong> both.<br />
Brief interventions by physicians have been found <strong>to</strong><br />
be effective <strong>with</strong> other conditions, including smoking<br />
cessation, improving dietary behavior, and reduction <strong>of</strong><br />
alcohol consumption. Thus, while data are limited on<br />
the <strong>to</strong>pic <strong>of</strong> <strong>HIV</strong> prevention, physicians should provide<br />
such counseling until studies suggest alternate and<br />
improved approaches.<br />
How can clinic staff other than the primary<br />
medical provider enhance <strong>HIV</strong> prevention<br />
practice?<br />
In most medium-sized and larger clinics, staff<br />
members other than the primary medical provider<br />
are responsible for referral, contact notification, and<br />
quality improvement, which can all be used <strong>to</strong> enhance<br />
prevention practice, as discussed below. In addition,<br />
specific structural interventions (eg, arranging client<br />
flow <strong>to</strong> ensure interaction <strong>with</strong> clinic staff who conduct<br />
prevention counseling, use <strong>of</strong> video, written handouts<br />
or other educational media, and distribution <strong>of</strong><br />
condoms) can strengthen the role <strong>of</strong> other clinic staff in<br />
prevention activities.<br />
What role does referral <strong>to</strong> community<br />
resources play in <strong>HIV</strong> prevention?<br />
Some complex patient issues and conditions fall<br />
beyond the scope <strong>of</strong> a primary care clinic and must<br />
be addressed before risky behavior can be reduced or<br />
eliminated. These include drug abuse, mental health<br />
issues, domestic violence, and assistance <strong>with</strong> needs<br />
such as housing, food, and employment. Each clinic<br />
should have established relationships <strong>with</strong> community<br />
resources <strong>to</strong> address these issues, and staff members<br />
should have thorough knowledge <strong>of</strong> the available<br />
services as well as mechanisms in place <strong>to</strong> ensure that<br />
patients can access the services. Finally, followup should<br />
be done <strong>to</strong> be certain that the referrals are utilized<br />
and are effective for each patient. It is unlikely that<br />
persons at highest risk for transmitting <strong>HIV</strong> <strong>to</strong> others<br />
can effectively reduce such behavior <strong>with</strong>out access <strong>to</strong> a<br />
comprehensive array <strong>of</strong> services and supports.<br />
What are key elements <strong>of</strong> contact notification?<br />
Contact notification is an effective way <strong>to</strong> identify<br />
additional <strong>HIV</strong>-infected persons through <strong>HIV</strong> counseling<br />
and testing, bring them in<strong>to</strong> care, and provide support<br />
<strong>to</strong> help them avoid transmitting <strong>HIV</strong> <strong>to</strong> others. Health<br />
departments traditionally conduct contact notification;<br />
in some States providers are required by law <strong>to</strong> report<br />
<strong>to</strong> the health department known sexual or drugequipment-sharing<br />
contacts <strong>of</strong> persons infected <strong>with</strong><br />
<strong>HIV</strong>. The standard method is <strong>to</strong> inform the patient’s<br />
contacts that they have been placed at risk and need<br />
<strong>HIV</strong> testing <strong>with</strong>out identifying the source.<br />
24<br />
U.S. Department <strong>of</strong> Health and Human Services, Health Resources and Services Administration, <strong>HIV</strong>/<strong>AIDS</strong> Bureau