Vol 43 # 2 June 2011 - Kma.org.kw
Vol 43 # 2 June 2011 - Kma.org.kw
Vol 43 # 2 June 2011 - Kma.org.kw
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
118<br />
KUWAIT MEDICAL JOURNAL<br />
<strong>June</strong> <strong>2011</strong><br />
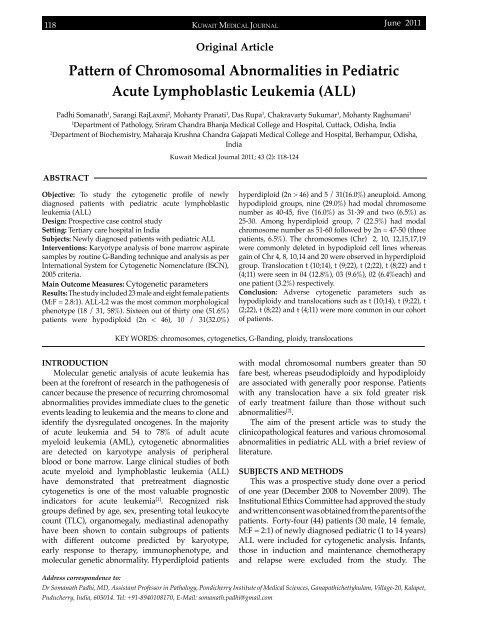
Original Article<br />
Pattern of Chromosomal Abnormalities in Pediatric<br />
Acute Lymphoblastic Leukemia (ALL)<br />
Padhi Somanath 1 , Sarangi RajLaxmi 2 , Mohanty Pranati 1 , Das Rupa 1 , Chakravarty Sukumar 1 , Mohanty Raghumani 1<br />
1<br />
Department of Pathology, Sriram Chandra Bhanja Medical College and Hospital, Cuttack, Odisha, India<br />
2<br />
Department of Biochemistry, Maharaja Krushna Chandra Gajapati Medical College and Hospital, Berhampur, Odisha,<br />
India<br />
Kuwait Medical Journal <strong>2011</strong>; <strong>43</strong> (2): 118-124<br />
ABSTRACT<br />
Objective: To study the cytogenetic profile of newly<br />
diagnosed patients with pediatric acute lymphoblastic<br />
leukemia (ALL)<br />
Design: Prospective case control study<br />
Setting: Tertiary care hospital in India<br />
Subjects: Newly diagnosed patients with pediatric ALL<br />
Interventions: Karyotype analysis of bone marrow aspirate<br />
samples by routine G-Banding technique and analysis as per<br />
International System for Cytogenetic Nomenclature (ISCN),<br />
2005 criteria.<br />
Main Outcome Measures: Cytogenetic parameters<br />
Results: The study included 23 male and eight female patients<br />
(M:F = 2.8:1). ALL-L2 was the most common morphological<br />
phenotype (18 / 31, 58%). Sixteen out of thirty one (51.6%)<br />
patients were hypodiploid (2n < 46), 10 / 31(32.0%)<br />
hyperdiploid (2n > 46) and 5 / 31(16.0%) aneuploid. Among<br />
hypodiploid groups, nine (29.0%) had modal chromosome<br />
number as 40-45, five (16.0%) as 31-39 and two (6.5%) as<br />
25-30. Among hyperdiploid group, 7 (22.5%) had modal<br />
chromosome number as 51-60 followed by 2n = 47-50 (three<br />
patients, 6.5%). The chromosomes (Chr) 2, 10, 12,15,17,19<br />
were commonly deleted in hypodiploid cell lines whereas<br />
gain of Chr 4, 8, 10,14 and 20 were observed in hyperdiploid<br />
group. Translocation t (10;14), t (9;22), t (2;22), t (8;22) and t<br />
(4;11) were seen in 04 (12.8%), 03 (9.6%), 02 (6.4%each) and<br />
one patient (3.2%) respectively.<br />
Conclusion: Adverse cytogenetic parameters such as<br />
hypodiploidy and translocations such as t (10;14), t (9;22), t<br />
(2;22), t (8;22) and t (4;11) were more common in our cohort<br />
of patients.<br />
KEY WORDS: chromosomes, cytogenetics, G-Banding, ploidy, translocations<br />
INTRODUCTION<br />
Molecular genetic analysis of acute leukemia has<br />
been at the forefront of research in the pathogenesis of<br />
cancer because the presence of recurring chromosomal<br />
abnormalities provides immediate clues to the genetic<br />
events leading to leukemia and the means to clone and<br />
identify the dysregulated oncogenes. In the majority<br />
of acute leukemia and 54 to 78% of adult acute<br />
myeloid leukemia (AML), cytogenetic abnormalities<br />
are detected on karyotype analysis of peripheral<br />
blood or bone marrow. Large clinical studies of both<br />
acute myeloid and lymphoblastic leukemia (ALL)<br />
have demonstrated that pretreatment diagnostic<br />
cytogenetics is one of the most valuable prognostic<br />
indicators for acute leukemia [1] . Recognized risk<br />
groups defined by age, sex, presenting total leukocyte<br />
count (TLC), <strong>org</strong>anomegaly, mediastinal adenopathy<br />
have been shown to contain subgroups of patients<br />
with different outcome predicted by karyotype,<br />
early response to therapy, immunophenotype, and<br />
molecular genetic abnormality. Hyperdiploid patients<br />
with modal chromosomal numbers greater than 50<br />
fare best, whereas pseudodiploidy and hypodiploidy<br />
are associated with generally poor response. Patients<br />
with any translocation have a six fold greater risk<br />
of early treatment failure than those without such<br />
abnormalities [2] .<br />
The aim of the present article was to study the<br />
clinicopathological features and various chromosomal<br />
abnormalities in pediatric ALL with a brief review of<br />
literature.<br />
SUBJECTS AND METHODS<br />
This was a prospective study done over a period<br />
of one year (December 2008 to November 2009). The<br />
Institutional Ethics Committee had approved the study<br />
and written consent was obtained from the parents of the<br />
patients. Forty-four (44) patients (30 male, 14 female,<br />
M:F = 2:1) of newly diagnosed pediatric (1 to 14 years)<br />
ALL were included for cytogenetic analysis. Infants,<br />
those in induction and maintenance chemotherapy<br />
and relapse were excluded from the study. The<br />
Address correspondence to:<br />
Dr Somanath Padhi, MD, Assistant Professor in Pathology, Pondicherry Institute of Medical Sciences, Ganapathichettykulam, Village-20, Kalapet,<br />
Puducherry, India, 605014. Tel: +91-8940108170, E-Mail: somanath.padhi@gmail.com