Vol 43 # 2 June 2011 - Kma.org.kw
Vol 43 # 2 June 2011 - Kma.org.kw
Vol 43 # 2 June 2011 - Kma.org.kw
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>June</strong> <strong>2011</strong><br />
KUWAIT MEDICAL JOURNAL 151<br />
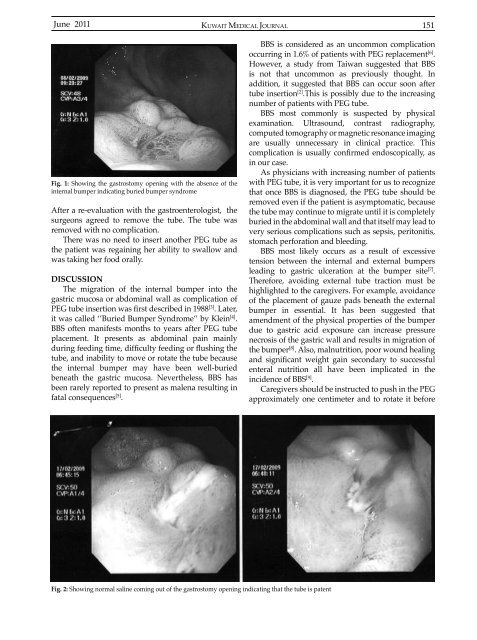
Fig. 1: Showing the gastrostomy opening with the absence of the<br />
internal bumper indicating buried bumper syndrome<br />
After a re-evaluation with the gastroenterologist, the<br />
surgeons agreed to remove the tube. The tube was<br />
removed with no complication.<br />
There was no need to insert another PEG tube as<br />
the patient was regaining her ability to swallow and<br />
was taking her food orally.<br />
DISCUSSION<br />
The migration of the internal bumper into the<br />
gastric mucosa or abdominal wall as complication of<br />
PEG tube insertion was first described in 1988 [3] . Later,<br />
it was called ‘’Buried Bumper Syndrome’’ by Klein [4] .<br />
BBS often manifests months to years after PEG tube<br />
placement. It presents as abdominal pain mainly<br />
during feeding time, difficulty feeding or flushing the<br />
tube, and inability to move or rotate the tube because<br />
the internal bumper may have been well-buried<br />
beneath the gastric mucosa. Nevertheless, BBS has<br />
been rarely reported to present as malena resulting in<br />
fatal consequences [5] .<br />
BBS is considered as an uncommon complication<br />
occurring in 1.6% of patients with PEG replacement [6] .<br />
However, a study from Taiwan suggested that BBS<br />
is not that uncommon as previously thought. In<br />
addition, it suggested that BBS can occur soon after<br />
tube insertion [2] .This is possibly due to the increasing<br />
number of patients with PEG tube.<br />
BBS most commonly is suspected by physical<br />
examination. Ultrasound, contrast radiography,<br />
computed tomography or magnetic resonance imaging<br />
are usually unnecessary in clinical practice. This<br />
complication is usually confirmed endoscopically, as<br />
in our case.<br />
As physicians with increasing number of patients<br />
with PEG tube, it is very important for us to recognize<br />
that once BBS is diagnosed, the PEG tube should be<br />
removed even if the patient is asymptomatic, because<br />
the tube may continue to migrate until it is completely<br />
buried in the abdominal wall and that itself may lead to<br />
very serious complications such as sepsis, peritonitis,<br />
stomach perforation and bleeding.<br />
BBS most likely occurs as a result of excessive<br />
tension between the internal and external bumpers<br />
leading to gastric ulceration at the bumper site [7] .<br />
Therefore, avoiding external tube traction must be<br />
highlighted to the caregivers. For example, avoidance<br />
of the placement of gauze pads beneath the external<br />
bumper in essential. It has been suggested that<br />
amendment of the physical properties of the bumper<br />
due to gastric acid exposure can increase pressure<br />
necrosis of the gastric wall and results in migration of<br />
the bumper [8] . Also, malnutrition, poor wound healing<br />
and significant weight gain secondary to successful<br />
enteral nutrition all have been implicated in the<br />
incidence of BBS [9] .<br />
Caregivers should be instructed to push in the PEG<br />
approximately one centimeter and to rotate it before<br />
Fig. 2: Showing normal saline coming out of the gastrostomy opening indicating that the tube is patent