Australasian Anaesthesia 2011 - Australian and New Zealand ...
Australasian Anaesthesia 2011 - Australian and New Zealand ...
Australasian Anaesthesia 2011 - Australian and New Zealand ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
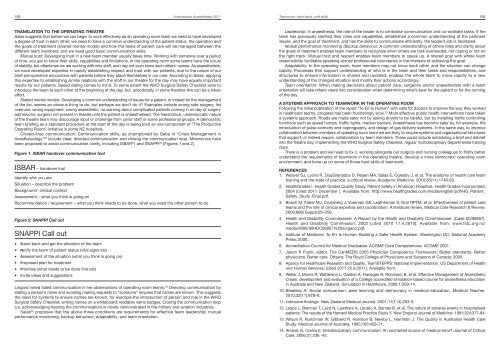
192 <strong>Australasian</strong> <strong>Anaesthesia</strong> <strong>2011</strong>Teamwork: hard facts, soft skills. 193TRANSLATION TO THE OPERATING THEATRESalas suggests that before we can begin to work effectively as an operating room team we need to have developeda degree of trust in each other; we need to have a common underst<strong>and</strong>ing of the patient status, the operation <strong>and</strong>the goals of treatment (shared mental model) <strong>and</strong> how the tasks of patient care will be managed between thedifferent team members; <strong>and</strong> we need good basic communication skills.Mutual trust: Developing trust in a new team member usually takes time. Working with someone over a periodof time, you get to know their skills, capabilities <strong>and</strong> limitations. In the operating room some teams have the luxuryof stability, but oftentimes we are working with new staff, <strong>and</strong> may not even know each others’ names. As anaesthetists,we have developed expertise in rapidly establishing respect <strong>and</strong> trust with our patients, due to the nature of ourbrief pre-operative encounters with patients before they place themselves in our care. According to Salas, applyingthis expertise to establishing similar relations with the staff in our theatre for the day may have equally importantresults for our patients. Speed dating comes to mind. To some extent the WHO Surgical Safety Checklist aims tointroduce the team to each other at the beginning of the day, but, anecdotally, in some theatres this can be a tokeneffort.Shared mental models: Developing a common underst<strong>and</strong>ing of issues for a patient, or indeed for the managementof the list, seems an obvious thing to do, but perhaps we don’t do it? Examples include wrong side surgery; listoverruns; wrong equipment; wrong anaesthetic; no warning about complicated patients coming in on day of surgeryadmissions; surgeon not present in theatre until the patient is anaesthetised. The hierarchical, undemocratic natureof the theatre team may discourage input or challenge from junior staff or some professional groups. A democraticteam briefing as a st<strong>and</strong>ard procedure at the start of the day is being tried as one component of “The ProductiveOperating Room” initiative in some NZ hospitals.Closed-loop communication: Communication skills, as championed by Gaba in “Crisis Management inAnesthesiology” 30 include clear, directed communication <strong>and</strong> closing the communication loop. Mnemonics havebeen proposed to assist communication clarity, including ISBAR 3 1 <strong>and</strong> SNAPPI 32 (Figures 1 <strong>and</strong> 2).Figure 1. ISBAR h<strong>and</strong>over communication toolISBAR – h<strong>and</strong>over toolIdentify who you areSituation – describe the problemBackground- clinical contextAssessment – what you think is going onRecommendation / requirement – what you think needs to be done, what you need the other person to doFigure 2: SNAPPI Call outSNAPPI Call out• St<strong>and</strong> back <strong>and</strong> get the attention of the team• Notify the team of patient status (vital signs etc)• Assessment of the situation (what you think is going on)• Proposed plan for treatment• Priorities (what needs to be done first etc)• Invite ideas <strong>and</strong> suggestionsLingard noted failed communication in her observations of operating room teams. 22 Directing communication bystating a person’s name <strong>and</strong> avoiding making requests to “someone” requires that names are known. This suggeststhe need for systems to ensure names are known, for example the introduction of person <strong>and</strong> role in the WHOSurgical Safety Checklist; writing names on a whiteboard; readable name badges. Closing the communication loop(i.e. acknowledging hearing the communication) is clearly demonstrated in the military <strong>and</strong> aviation industries.Salas 29 proposes that the above three conditions are requirements for effective team leadership; mutualperformance monitoring; backup behaviour; adaptability; <strong>and</strong> team orientation.Leadership: In anaesthesia, the role of the leader is to centralise communication <strong>and</strong> co-ordinate tasks. If theteam has previously clarified their roles <strong>and</strong> capabilities, established a common underst<strong>and</strong>ing of the pertinentissues, <strong>and</strong> the goal of treatment, <strong>and</strong> has the skills to communicate efficiently, the leader’s job is facilitated.Mutual performance monitoring /Backup behaviour: A common underst<strong>and</strong>ing of others roles <strong>and</strong> clarity aboutthe goals of treatment enables team members to recognise when others are task overloaded, not coping or not onthe right track. Mutual trust <strong>and</strong> respect enables team members to speak up. A shared goal with whole teamresponsibility facilitates speaking across professional boundaries in the interests of achieving the goal.Adaptability: In the operating room, team members may not know each other, <strong>and</strong> the situation can changerapidly. Processes that support underst<strong>and</strong>ing of who is in the team <strong>and</strong> their tasks <strong>and</strong> responsibilities, <strong>and</strong>structures to ensure information is shared <strong>and</strong> updated, enables the whole team to move rapidly to a newunderst<strong>and</strong>ing of the changed situation <strong>and</strong> modify their actions accordingly.Team orientation: When making decisions about patient care, surgeons <strong>and</strong>/or anaesthetists with a teamorientation will take others views into consideration when determining what’s best for the patient or for the runningof the day.A SYSTEMS APPROACH TO TEAMWORK IN THE OPERATING ROOMFollowing the initial publication of the report “To Err is Human” with calls for doctors to improve the way they workedin healthcare teams, progress has been frustratingly slow. 33 Most effective public health interventions have takena systems approach. Roads are made safer not by asking drivers to be careful, but by installing traffic controllingfunctions such as speed humps, traffic lights, median barriers. <strong>Anaesthesia</strong> has become safer by, for example, theintroduction of pulse oximetry <strong>and</strong> capnography, <strong>and</strong> design of gas delivery systems. In the same way, to improvecollaboration between members of operating room team we are likely to require systems <strong>and</strong> organisational structuresthat support, or indeed require, collaboration by team members. These could include scheduling a brief <strong>and</strong> debriefinto the theatre day, implementing the WHO Surgical Safety Checklist, regular multidisciplinary departmental trainingdays.There is a problem <strong>and</strong> we need to fix it, working alongside our surgical <strong>and</strong> nursing colleagues to firstly betterunderst<strong>and</strong> the requirements of teamwork in the operating theatre, develop a more democratic operating roomenvironment, <strong>and</strong> hone up on some of those hard skills of teamwork.REFERENCES1. Weaver SJ, Lyons R, DiazGranados D, Rosen MA, Salas E, Oglesby J, et al. The anatomy of health care teamtraining <strong>and</strong> the state of practice: a critical review. Academic Medicine. 2010;85(11):1746-60.2. HealthGrades I. Health Grades Quality Study. Patient Safety in American Hospitals. Health Grades Incorporated;2004 [cited <strong>2011</strong> December ]. Available from: http://www.healthgrades.com/media/english/pdf/HG_Patient_Safety_Study_Final.pdf.3. Bosch M, Faber MJ, Cruijsberg J, Voerman GE, Leatherman S, Grol RPTM, et al. Effectiveness of patient careteams <strong>and</strong> the role of clinical expertise <strong>and</strong> coordination: A literature review. Medical Care Research & Review.2009;66(6 Suppl):5S-35S.4. Health <strong>and</strong> Disability Commissioner. A Report by the Health <strong>and</strong> Disability Commissioner. (Case 00/06857).Health <strong>and</strong> Disability Commission; 2002 [cited 2010 17.4.2010]. Available from: www.hdc.org.nz/media/2695/00HDC06857%20surgeon.pdf.5. Institute of Medicine. To Err Is Human: Building a Safer Health System. Washington DC: National AcademyPress; 2000.6. Accreditation Council for Medical Graduates. ACGME Core Competencies. ACGME 2001.7. Jason R Frank, editor. The CanMEDS 2005 Physician Competency Framework: Better st<strong>and</strong>ards. Betterphysicians. Better care. Ottawa: The Royal College of Physicians <strong>and</strong> Surgeons of Canada; 2005.8. Agency for Healthcare Research <strong>and</strong> Quality. TeamSTEPPS: National Implementation. US Department of Health<strong>and</strong> Human Services; [cited <strong>2011</strong> 22.9.<strong>2011</strong>]. Available from.9. Weller J, Morris R, Watterson L, Garden A, Flanagan B, Robinson B, et al. Effective Management of AnaestheticCrises: development <strong>and</strong> evaluation of a College accredited simulation-based course for anaesthesia educationin Australia <strong>and</strong> <strong>New</strong> Zeal<strong>and</strong>. Simulation in Healthcare. 2006;1:209-14.10. Bleakley A. Social comparison, peer learning <strong>and</strong> democracy in medical education. Medical Teacher.2010;32(11):878-9.11. indicative findings. <strong>New</strong> Zeal<strong>and</strong> Medical Journal. 2001;11(114):203-5.12. Leape L, Brennan T, Laird N, Lawthers A, Localio A, Barnes B, et al. The nature of adverse events in hospitalisedpatients: The results of the Harvard Medical Practice Study II. <strong>New</strong> Engl<strong>and</strong> Journal of Medicine. 1991;324:377-84.13. Wilson R, Runciman W, Gibberd R, Harrison B, <strong>New</strong>by L, Hamilton J. The Quality in <strong>Australian</strong> Health CareStudy. Medical Journal of Australia. 1995;163:458-71.14. Alvarez G, Coiera E. Interdisciplinary communication: An uncharted source of medical error? Journal of CriticalCare. 2006;21:236 -42.