Australasian Anaesthesia 2011 - Australian and New Zealand ...
Australasian Anaesthesia 2011 - Australian and New Zealand ...
Australasian Anaesthesia 2011 - Australian and New Zealand ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
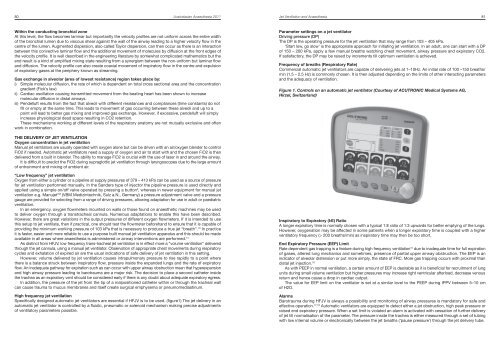
80 <strong>Australasian</strong> <strong>Anaesthesia</strong> <strong>2011</strong>Jet Ventilation <strong>and</strong> <strong>Anaesthesia</strong> 81Within the conducting bronchial zoneAt this level, the flow becomes laminar but importantly the velocity profiles are not uniform across the entire widthof the bronchial lumen due to viscous shear against the wall of the airway leading to a higher velocity flow in thecentre of the lumen. Augmented dispersion, also called Taylor dispersion, can then occur as there is an interactionbetween this convective laminar flow <strong>and</strong> the additional movement of molecules by diffusion at the front edges ofthe velocity profile. It is well described in the engineering literature by somewhat complicated mathematics but theend result is a kind of amplified mixing state resulting from a synergism between the non-uniform but laminar flow<strong>and</strong> diffusion. The velocity profile can also create coaxial movement of inspiratory flow in the centre <strong>and</strong> expulsionof expiratory gases at the periphery known as streaming.Gas exchange in alveolar (area of lowest resistance) region takes place by:i) Simple molecular diffusion, the rate of which is dependent on total cross sectional area <strong>and</strong> the concentrationgradient (Fick’s law)ii) Cardiac oscillation causing transmitted movement from the beating heart has been shown to increasemolecular diffusion in distal airways.iii) Pendelluft results from the fact that alveoli with different resistances <strong>and</strong> compliances (time constants) do notfill or empty at the same time. This leads to movement of gas occurring between these alveoli <strong>and</strong> up to apoint will lead to better gas mixing <strong>and</strong> improved gas exchange. However, if excessive, pendelluft will simplyincrease physiological dead space resulting in CO2 retention.These mechanisms working at different levels of the respiratory anatomy are not mutually exclusive <strong>and</strong> oftenwork in combination.Parameter settings on a jet ventilatorDriving pressure (DP)The DP is the operating pressure for the jet ventilation that may range from 103 – 405 kPa.‘Start low, go slow’ is the appropriate approach for initiating jet ventilation. In an adult, one can start with a DPof 150 – 200 kPa, apply a few manual breaths watching chest movement, airway pressure <strong>and</strong> expiratory CO2.If satisfactory, the DP may be raised by increments till optimum ventilation is achieved.Frequency of breaths (Respiratory Rate)Commercial automatic jet ventilators are capable of delivering jets at 1–10Hz. An initial rate of 100 –150 breaths/min (1.5 – 2.5 Hz) is commonly chosen. It is then adjusted depending on the limits of other interacting parameters<strong>and</strong> the adequacy of ventilation.Figure 1. Controls on an automatic jet ventilator (Courtesy of ACUTRONIC Medical Systems AG,Hirzel, Switzerl<strong>and</strong>)THE DELIVERY OF JET VENTILATIONOxygen concentration in jet ventilationManual jet ventilators are usually operated with oxygen alone but can be driven with an air/oxygen blender to controlFiO2 if needed. Automatic jet ventilators need a supply of oxygen <strong>and</strong> air to start with <strong>and</strong> the chosen FiO2 is thendelivered from a built in blender. The ability to manage FiO2 is crucial with the use of laser in <strong>and</strong> around the airway.It is difficult to predict the FiO2 during supraglottic jet ventilation through laryngoscopes due to the large amountof entrainment <strong>and</strong> mixing of ambient air.“Low frequency” jet ventilationOxygen from either a cylinder or a pipeline at supply pressures of 379 – 413 kPa can be used as a source of pressurefor jet ventilation performed manually. In the S<strong>and</strong>ers type of injector the pipeline pressure is used directly <strong>and</strong>applied using a simple on/off valve operated by pressing a button 3 , whereas in newer equipment for manual jetventilation e.g. Manujet TM (VBM Medizintechnik, Sulz a.N., Germany) a pressure adjustment valve <strong>and</strong> a pressuregauge are provided for selecting from a range of driving pressures, allowing adaptation for use in adult or paediatricventilation.In an emergency, oxygen flowmeters mounted on walls or those found on anaesthetic machines may be usedto deliver oxygen through a transtracheal cannula. Numerous adaptations to enable this have been described.However, there are great variations in the output pressures of different oxygen flowmeters. If it is intended to usethis setup to jet ventilate, then if practical, one should test the flowmeter beforeh<strong>and</strong> to ensure that it is capable ofproviding the minimum working pressure of 103 kPa that is necessary to produce a true jet “breath”. 13 In practiceit is faster, easier <strong>and</strong> more reliable to use a purpose built manual jet ventilation apparatus <strong>and</strong> this should be madeavailable in all areas where anaesthesia is administered or airway interventions are performed. 14As distinct from HFJV, low frequency trans-tracheal jet ventilation is in effect more a “volume ventilation” deliveredthrough the jet cannula, using a manual jet ventilator. Observation of appropriate chest movements during respiratorycycles <strong>and</strong> exhalation of expired air are the usual indications of safe delivery of jet ventilation in this setting.However, volume delivered by jet ventilation causes intrapulmonary pressure to rise rapidly to a point wherethere is a balance struck between inspiratory flow, pressure inside the exp<strong>and</strong>ed lungs <strong>and</strong> the rate of expiratoryflow. An inadequate pathway for expiration such as can occur with upper airway obstruction mean that hyperexpansion<strong>and</strong> high airway pressure leading to barotrauma are a major risk. The decision to place a second catheter insidethe trachea as an expiratory vent should be considered early if there is any doubt about adequate expiratory egress.In addition, the pressure of the jet from the tip of a malpositioned catheter within or through the tracheal wallcan cause trauma to mucus membranes <strong>and</strong> itself create surgical emphysema or pneumomediastinum.High frequency jet ventilationSpecifically designed automatic jet ventilators are essential if HFJV is to be used. (figure1) The jet delivery in anautomatic jet ventilator is controlled by a fluidic, pneumatic or solenoid mechanism making precise adjustmentsof ventilatory parameters possible.Inspiratory to Expiratory (I:E) RatioA longer expiratory time is normally chosen with a typical 1:E ratio of 1:3 upwards for better emptying of the lungs.However, oxygenation may be affected in some patients when a longer expiratory time is coupled with a higherventilatory frequency (> 200 breaths/min) as inspiratory time may then be too short.End Expiratory Pressure (EEP) LimitRate dependent gas trapping is a feature during high frequency ventilation 15 due to inadequate time for full expirationof gases, altered lung mechanics <strong>and</strong> sometimes, presence of partial upper airway obstruction. The EEP is anindicator of alveolar distension or put more simply, the state of FRC. More gas trapping occurs with proximal th<strong>and</strong>istal jet injection. 16As with PEEP in normal ventilation, a certain amount of EEP is desirable as it is beneficial for recruitment of lungunits during small volume ventilation but higher pressures may increase right ventricular afterload, decrease venousreturn <strong>and</strong> hence cause a drop in cardiac output.The value for EEP limit on the ventilator is set at a similar level to the PEEP during IPPV between 5–10 cmof H2O.AlarmsBarotrauma during HFJV is always a possibility <strong>and</strong> monitoring of airway pressures is m<strong>and</strong>atory for safe <strong>and</strong>effective operation. 17,18 Automatic ventilators are equipped to detect either a jet obstruction, high peak pressure orraised end expiratory pressure. When a set limit is violated an alarm is activated with cessation of further deliveryof jet till normalisation of the parameter. The pressure inside the trachea is either measured through a set of tubingwith low internal volume or electronically between the jet breaths (‘pause pressure’) through the jet delivery tube.