160 <strong>Australasian</strong> <strong>Anaesthesia</strong> <strong>2011</strong>Oxytocin: A guide for Anaesthetists 161AnaphylaxisThere are numerous case reports implicating Syntocinon as the cause of an allergic reaction but few where thisreaction has been confirmed by skin testing. Oxytocin is a skin irritant if injected subcutaneously. It has beenpostulated that some of the cases of allergy attributed to syntocinon were more likely to have been a reaction dueto latex. 29CARBETOCINCarbetocin is a synthetic analogue of oxytocin, with structural modifications. These modifications protect thecarbetocin molecule from degradation by oxytocinase, therefore prolonging its half-life <strong>and</strong> pharmacological effect.Carbetocin (Duratocin, Ferring) is supplied in a 1 mL ampoule, containing 100 micrograms of the drug, which is therecommended bolus dose when administered intravenously or intramuscularly. 30The half-life of Carbetocin is approximately 40 minutes after an intravenous injection. The tonic uterine activityis 60 minutes after intravenous injection <strong>and</strong> 120 minutes after intramuscular injection. There have been minimaladverse effects associated with carbetocin’s use <strong>and</strong> its side effect rate is likely similar to Syntocinon. 31A Cochrane Review from 2007 looked at four studies (three at caesarean delivery <strong>and</strong> one at vaginal delivery)that compared carbetocin to Syntocinon to prevent postpartum haemorrhage. Carbetocin resulted in a statisticallysignificant reduction in the need for therapeutic uterotonic agents (in the caesarean delivery groups), but there wasinsufficient evidence that carbetocin was as effective as Syntocinon to prevent postpartum haemorrhage. Therewas no significant reduction in need for therapeutic uterotonic drugs after vaginal delivery. There was no differencein adverse events. 32The proposed advantages of carbetocin over Syntocinon are its longer half-life <strong>and</strong> the subsequent need for asingle IV or IM injection, rather than an infusion. Further studies looking at its effect in cardiac patients, women withpre-eclampsia <strong>and</strong> in women already bleeding are required.SUMMARYSyntocinon remains an important drug for the prevention <strong>and</strong> treatment of post partum haemorrhage. The evidencesupporting injection of a 5 IU dose at delivery is scant <strong>and</strong> this dose causes transient but profound cardiovascularside effects when given as a rapid bolus. Recent studies suggest that a smaller dose at both elective <strong>and</strong> nonelectivecaesarean delivery is sufficient to improve uterine tone, <strong>and</strong> these doses potentially reduce the severity ofhaemodynamic side effects.The international guidelines for the dosage of Syntocinon after caesarean delivery are varied. There are alsowarnings about this drug, both with a black box warning from the United States FDA 33 <strong>and</strong> inclusion on a list ofhigh alert medications from the Institute for Safe Medication Practices .34The haemodynamic effects of a 5 IU bolus are unlikely to cause significant problems in healthy women, but itseems appropriate to use a lower dose of 2-3 IU bolused slowly <strong>and</strong> titrate further doses to effect. An editorialpublished in 2010 in the International Journal of Obstetric <strong>Anaesthesia</strong> recommends an initial dose of less than5IU, as a slow bolus. 35 It is encouraging to know that smaller doses result in adequate uterine tone in women withcardiac conditions or hypovolaemia who are unable to produce a compensatory increase in cardiac output.A recent study by King <strong>and</strong> colleagues 23 also suggests that an initial high dose infusion, rather than a bolus,produces satisfactory uterine tone. Unfortunately, this study was not powered to assess side effects from the highdose initial infusion. An adequate <strong>and</strong> safe dose rate of Sytnocinon by infusion post delivery is yet to be clarified.It is important to remember women with prolonged labour prior to presenting for caesarean delivery <strong>and</strong> thosereceiving a Syntocinon infusion prior to delivery are likely to require a higher dose of Syntocinon. They may alsorequire other uterotonic drugs that act on the myometrium via other mechanisms, such as Ergomterine or Misoprostol.The present data supports a dose of 2 IU given as a slow bolus for elective caesarean sections, with an increaseto a 3 IU bolus for non-elective caesarean deliveries. These women should receive infusions post delivery.What is not clear at the present time, is the most suitable dose of Syntocinon in the context of a generalanaesthetic, particularly when using volatile agents which relax the myometrium. It has not been established whatbolus doses or infusion rates should be used in women who have more than one risk factor for uterine atony, otherrisk factors for post partum haemorrhage or women with pre-eclampsia.REFERENCES1. Saving Mothers’ Lives: Reviewing maternal deaths to make motherhood safer: 2006–2008. The Eighth Reportof the Confidential Enquiries into Maternal Deaths in the United Kingdom. British Journal of Obstetrics <strong>and</strong>Gynaecology, <strong>2011</strong>. 118, supplement 1.2. Sullivan, E., B. Hall, <strong>and</strong> J. King, Maternal Deaths in Australia 2003-2005, 2008, <strong>Australian</strong> Government: <strong>Australian</strong>Institute of Health <strong>and</strong> Welfare.3. Al-Zirqi, I., et al., Prevalence <strong>and</strong> risk factors of severe obstetric haemorrhage. BJOG : an international journalof obstetrics <strong>and</strong> gynaecology, 2008. 115(10): p. 1265-72.4. Why Mothers DIe. Report on Confidential Enquiries into Maternal Deaths in the United Kingdom 1997 – 1999,in Royal College of Obstetricians <strong>and</strong> Gynaecologists2001, London.5. Du Vigneaud, V., et al., Oxytocin: Synthesis. Journal of the American Chemical Society, 1954. 76(12): p. 3115–3118.6. http://www.nobelprize.org.7. Prendiville, W., The effect of routine oxytocic administration in the management of the third stage of labour: anoverview of the evidence from controlled trials. British Journal of Obstetrics <strong>and</strong> Gynaecology, 1988. 95: p. 3-16.8. Gimpl, G. <strong>and</strong> F. Fahrenholz, The Oxytocin Receptor System: Structure, Function <strong>and</strong> Regulation. PhysiologicalReviews, 2001. 81(2): p. 629-683.9. Harrison’s: Principles of Internal Medicine. 17th. ed, ed. B. Fauci, Kasper, Hauser, Longo, Jameson,Loscalzo.2008, <strong>New</strong> York.: McGraw Hill Medical.10. Fuchs, A., et al., Oxytocin receptors in the human uterus during pregnancy <strong>and</strong> partuition. American Journal ofObstetrics <strong>and</strong> Gynaecology, 1984. 150: p. 734-41.11. Wray, S., Uterine contraction <strong>and</strong> physiological mechanism of modulation. American Journal of Physiology,1993(264): p. C1-18.12. Sasada, M. <strong>and</strong> S. Smith, Drugs in <strong>Anaesthesia</strong> <strong>and</strong> Intensive Care. Third Edition ed2003, <strong>New</strong> York: OxfordUniversity Press.13. Novartis Drug Pamphlet: Syntocinon, in Novartis Pharmaceuticals Australia Pty. Ltd.2009.14. Mathur, V.S. <strong>and</strong> J.M. Walker, Oxytocinase in Plasma <strong>and</strong> Placenta in normal <strong>and</strong> prolonged labour. BritishMedical Journal, 1968. 3: p. 96-97.15. Rosaeg, O.P., N.J. Cicutti, <strong>and</strong> R.S. Labow, The effect of oxytocin on the contractile force of human atrialtrabeculae. Anesthesia <strong>and</strong> analgesia, 1998. 86(1): p. 40-4.16. http://www.bnf.org.17. http://www.rcog.org.uk.18. Mockler, J.C., D.J. Murphy, <strong>and</strong> E.M. Wallace, An <strong>Australian</strong> <strong>and</strong> <strong>New</strong> Zeal<strong>and</strong> survey of practice of the useof oxytocin at elective caesarean section. The <strong>Australian</strong> & <strong>New</strong> Zeal<strong>and</strong> journal of obstetrics & gynaecology,2010. 50(1): p. 30-5.19. Sartain, J.B., et al., Intravenous oxytocin bolus of 2 units is superior to 5 units during elective Caesarean section.British journal of anaesthesia, 2008. 101(6): p. 822-6.20. Carvalho, J.C., et al., Oxytocin requirements at elective cesarean delivery: a dose-finding study. Obstetrics <strong>and</strong>gynecology, 2004. 104(5 Pt 1): p. 1005-10.21. Butwick, A.J., et al., Minimum effective bolus dose of oxytocin during elective Caesarean delivery. British journalof anaesthesia, 2010. 104(3): p. 338-43.22. Secher, N.J., P. Arnsbo, <strong>and</strong> L. Wallin, Haemodynamic effects of oxytocin (syntocinon) <strong>and</strong> methyl ergometrine(methergin) on the systemic <strong>and</strong> pulmonary circulations of pregnant anaesthetized women. Acta obstetricia etgynecologica Sc<strong>and</strong>inavica, 1978. 57(2): p. 97-103.23. King, K., et al., Five Unit Bolus Oxytocin at Cesarean Delivery in Women at Risk of Atony: A r<strong>and</strong>omized, Double-Blind, Controlled trial. Anesthesia <strong>and</strong> analgesia, 2010. 111: p. 1460-1466.24. Why Mothers Die. Report on Confidential Enquiries into Maternal Deaths in the United Kingdom 2003-2005.Royal College of Obstetricians <strong>and</strong> Gynaecologists, 2007.25. Mukaddam-Daher, S., et al., Negative inotropic <strong>and</strong> chronotropic effects of oxytocin. Hypertension, 2001. 38(2):p. 292-6.26. Pinder, A., et al., haemodynamic changes caused by oxytoxin during caesarean section under spinal anaesthesia.International Journal of Obstetric <strong>Anaesthesia</strong>, 2002. 11: p. 156-159.27. Svanstrom, M., et al., Signs of myocardial ischaemia after injection of oxytocin: a r<strong>and</strong>omised double-blindcomparison of oxytocin <strong>and</strong> methylergometrine during caesarean delivery. British journal of anaesthesia, 2008.100(5): p. 683-9.28. Jonsson, M., et al., ST depression at caesarean section <strong>and</strong> teh relation to oxytocin dose. A r<strong>and</strong>omised controlledtrial. British Journal of Obstetrics <strong>and</strong> Gynaecology, 2009. 117: p. 76-83.29. Schnider <strong>and</strong> Levinson’s Anesthesia for Obstetrics. 4th edition ed, ed. L.G. Hughes S, Rosen M.2002, Philadelphie:Lippincott Williams & Wilkins.30. Duratocin: Carbetocin. Single injection for lasting prevention, F.P.P. Ltd, Editor.31. Werner, R., Prevention of postpartum haemorrhage with the oxytocin analogue carbetocin. European Journalof Obstetrics & Gynecology <strong>and</strong> Reproductive Biology, 2009. 147(1): p. 15-20.32. Su, L.L., Y.S. Chong, <strong>and</strong> M. Samuel, Oxytocin agonists for preventing postpartum haemorrhage. The CochraneDatabase of Systematic Reviews, 2007(3).33. Formweb. FDA Black Box Warnings. http://www.blackboxrx.com/app/display.php?id=277.34. Practices, I.f.S.M. High Alert Medications. http://www.ismp.org 2010.35. Tsen, L. <strong>and</strong> M. Balki, Oxytocin Protocols during Cesarean Delivery: time to acknowledge the risk/benefit ration?International Journal of Obstetric <strong>Anaesthesia</strong>, 2010. 19: p. 243-245.
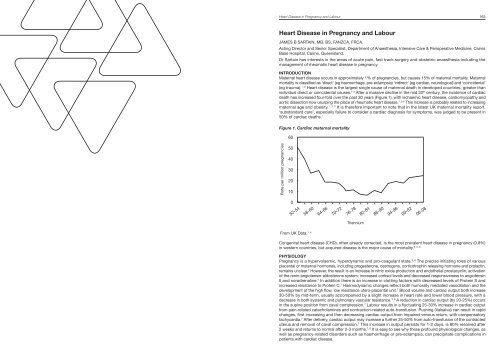
Heart Disease in Pregnancy <strong>and</strong> Labour 163Heart Disease in Pregnancy <strong>and</strong> LabourJAMES B SARTAIN, MB, BS, FANZCA, FRCA.Acting Director <strong>and</strong> Senior Specialist, Department of <strong>Anaesthesia</strong>, Intensive Care & Perioperative Medicine, CairnsBase Hospital, Cairns, Queensl<strong>and</strong>.Dr Sartain has interests in the areas of acute pain, fast track surgery <strong>and</strong> obstetric anaesthesia including themanagement of rheumatic heart disease in pregnancy.INTRODUCTIONMaternal heart disease occurs in approximately 1% of pregnancies, but causes 15% of maternal mortality. Maternalmortality is classified as ‘direct’ (eg haemorrhage, pre-eclampsia) ‘indirect’ (eg cardiac, neurological) <strong>and</strong> ‘coincidental’(eg trauma). 1, 2 Heart disease is the largest single cause of maternal death in developed countries, greater thanindividual direct or coincidental causes. 1-3 After a massive decline in the mid 20 th century, the incidence of cardiacdeath has increased four-fold over the past 30 years (Figure 1), with ischaemic heart disease, cardiomyopathy <strong>and</strong>aortic dissection now usurping the place of rheumatic heart disease. 1, 3-6 This increase is probably related to increasingmaternal age <strong>and</strong> obesity. 1, 3, 5 It is therefore important to note that in the latest UK maternal mortality report,‘subst<strong>and</strong>ard care’, especially failure to consider a cardiac diagnosis for symptoms, was judged to be present in50% of cardiac deaths. 1Figure 1. Cardiac maternal mortality60Rate per million pregnancies5040302010052-5458-6064-6670-7276-7882-8486-9094-9600-0206-08TrienniumFrom UK Data. 1, 4Congenital heart disease (CHD), often already corrected, is the most prevalent heart disease in pregnancy (0.8%)3, 5, 6in western countries, but acquired disease is the major cause of mortality.PHYSIOLOGYPregnancy is a hypervolaemic, hyperdynamic <strong>and</strong> pro-coagulant state. 3, 6 The precise initiating roles of variousplacental or maternal hormones, including progesterone, oestrogens, corticotrophin releasing hormone <strong>and</strong> prolactin,remains unclear. 7 However, the result is an increase in nitric oxide production <strong>and</strong> endothelial prostacyclin; activationof the renin-angiotensin-aldosterone system; increased cortisol levels <strong>and</strong> decreased responsiveness to angiotensinII <strong>and</strong> noradrenaline. 7 In addition there is an increase in clotting factors with decreased levels of Protein S <strong>and</strong>increased resistance to Protein C. 7 Haemodynamic changes reflect both humorally mediated vasodilation <strong>and</strong> thedevelopment of the high flow, low resistance utero-placental unit. 7 Blood volume <strong>and</strong> cardiac output both increase30-50% by mid-term, usually accompanied by a slight increase in heart rate <strong>and</strong> lower blood pressure, with adecrease in both systemic <strong>and</strong> pulmonary vascular resistance. 3, 6 A reduction in cardiac output (by 20-25%) occursin the supine position from caval compression. 7 Labour results in a fluctuating 25-30% increase in cardiac outputfrom pain-related catecholamines <strong>and</strong> contraction-related auto-transfusion. Pushing (Valsalva) can result in rapidchanges, first increasing <strong>and</strong> then decreasing cardiac output from impaired venous return, with compensatorytachycardia. 7 After delivery, cardiac output may increase a further 25-50% from auto-transfusion of the contracteduterus <strong>and</strong> removal of caval compression. 7 This increase in output persists for 1-2 days, is 80% resolved after2 weeks <strong>and</strong> returns to normal after 2-3 months. 7, 8 It is easy to see why these profound physiological changes, aswell as pregnancy-related disorders such as haemorrhage or pre-eclampsia, can precipitate complications inpatients with cardiac disease.