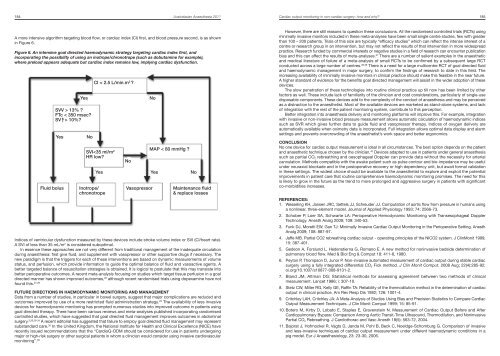
184 <strong>Australasian</strong> <strong>Anaesthesia</strong> <strong>2011</strong>Cardiac output monitoring in non-cardiac surgery: how <strong>and</strong> why? 185However, there are still reasons to question these conclusions. All the r<strong>and</strong>omised controlled trials (RCTs) usingA more intensive algorithm targeting blood flow, or cardiac index (CI) first, <strong>and</strong> blood pressure second, is as shownminimally invasive monitors included in these meta-analyses have been small single centre studies, few with greaterin Figure 6.than 100 – 200 patients. Trials of this size are typically “efficacy studies” which can reflect the intense interest of acentre or research group in an intervention, but may not reflect the results of that intervention in more widespreadFigure 6. An intensive goal directed haemodynamic strategy targeting cardiac index first, <strong>and</strong>practice. Research funded by commercial interests or negative studies in a field of research can encounter publicationincorporating the possibility of using an inotrope/chronotrope (such as dobutamine for example),bias <strong>and</strong> this can affect the results of meta-analyses. 37 There are a number of salient examples in the anaestheticwhere preload appears adequate but cardiac index remains low, implying cardiac dysfunction.<strong>and</strong> medical literature of failure of a meta-analysis of small RCTs to be confirmed by a subsequent large RCTconducted across a large number of centres. 38,39 There is a need for a large multicentre RCT of goal directed fluid<strong>and</strong> haemodynamic management in major surgery, to confirm the findings of research to date in this field. Theincreasing availability of minimally invasive monitors in clinical practice should make this feasible in the near future.A higher st<strong>and</strong>ard of evidence for the benefits goal directed management will assist in the wider adoption of theseCI < 2.5 L/min.m 2 ?devices.The slow penetration of these technologies into routine clinical practice up till now has been limited by otherYesSVV > 13% ?FTc < 350 msec?SV |^> 10%?Nofactors as well. These include lack of familiarity of the clinician <strong>and</strong> cost considerations, particularly of single-usedisposable components. These devices add to the complexity of the conduct of anaesthesia <strong>and</strong> may be perceivedas a distraction to the anaesthetist. Most of the available devices are marketed as st<strong>and</strong>-alone systems, <strong>and</strong> lackof integration with the rest of the patient monitoring system, contribute to this perception.Better integration into anaesthesia delivery <strong>and</strong> monitoring platforms will improve this. For example, integrationwith invasive or non-invasive blood pressure measurement allows automatic calculation of haemodynamic indicessuch as SVR which gives further data to guide fluid <strong>and</strong> vasopressor therapy. Indices of oxygen delivery areautomatically available when oximetry data is incorporated. Full integration allows optimal data display <strong>and</strong> alarmYesNoSVI
186 <strong>Australasian</strong> <strong>Anaesthesia</strong> <strong>2011</strong>Cardiac output monitoring in non-cardiac surgery: how <strong>and</strong> why? 18712. Peyton P, Chong SW. Minimally invasive measurement of cardiac output during surgery <strong>and</strong> critical care:A meta-analysis of accuracy <strong>and</strong> precision. Anesthesiology, 2010; 113 (5): 1220-35.13. Runciman, W. B., A. H. Ilsley, J. G. Roberts. Thermodilution cardiac output – a systematic error. Anaesth IntensCare 9: 135-9, 1981.14. Tournadre, J.P., D. Chassard <strong>and</strong> R. Muchada. Overestimation of low cardiac output measured by thermodilution.Br J Anaesth 79: 514-6, 1997.15. Van Grondelle, A., R. V. Ditchey, B. M. Groves, W. W. Wagner <strong>and</strong> J. T. Reeves. Thermodilution methodoverestimates low cardiac output in humans. Am J Physiol (Heart Circ Physiol) 14: H690-2, 1983.16. Bein B, Renner J, Scholz J, Tonner PH: Comparing different methods of cardiac output determination: A callfor consensus. Eur J Anaesthesiol 2006; 23: 710.17. Linton NWF, Linton RA, Della Rocca G, Costa MG: Is comparison of changes in cardiac output, assessed bydifferent methods, better than only comparing cardiac output to the reference method? Br J Anaesth 2002;89: 336-7.18. Feldman JM: Is It a Bird? Is It a Plane? The Role of Patient Monitors in Medical Decision Making. Anesth Analg2009; 108: 707-10.19. Critchley LA, Yang XX, Lee A. Assessment of Trending Ability of Cardiac Output Monitors by Polar PlotMethodology. J J Cardiothorac Vasc Anesth <strong>2011</strong>; 25(3): 536-546.20. Bein B, Meybohm P, Carvus E, Renner J, Tonner P, Steinfath M, Scholz J, Doerges V. The Reliability of PulseContour-Derived Cardiac Output During Hemorrhage <strong>and</strong> After Vasopressor Administration. Anesth Analg, 105(1): 107-13, 2007.21. Collange O, Xavier L, Kuntzman H, Calon B, Schaeffer R, Pottecher T, Diemunsch P, Pessaux P. FloTrac formonitoring arterial pressure <strong>and</strong> cardiac output during phaeochromocytoma surgery. Eur J Anaesthesiology.25: 779-80, 2008.22. Vannucci A, Krejci V, Kangrga I: Performance of Vigileo <strong>and</strong> LiDCOplus cardiac output monitors during a prolongedcardiac arrest <strong>and</strong> resuscitation. Eur J Anaesthesiol 2009; 26: 885-7.23. Marik PE, Cavallazzi R, Vasu T, Hirani A. Dynamic changes in arterial waveform derived variables <strong>and</strong> fluidresponsiveness in mechanically ventilated patients: a systematic review of the literature. Crit Care Med2009;37:2642–7.24. Bendjelid K, Rom<strong>and</strong> JA. Fluid responsiveness in mechanically ventilated patients: a review of indices used inintensive care. Intensive Care Med 2003; 29:352-360.25. Kungys G, Rose DD, Fleming NW. Stroke Volume Variation During Acute Normovolemic Hemodilution. AnesthAnalg 2009;109:1823–30.26. Gurgel ST, do Nascimento P Jr. Maintaining tissue perfusion in high-risk surgical patients: a systematic reviewof r<strong>and</strong>omized clinical trials. Anesth Analg <strong>2011</strong>; 112:1384-91.27. Davies SJ, David Yates D, Wilson RJT. Dopexamine Has No Additional Benefit in High-Risk Patients ReceivingGoal-Directed Fluid Therapy Undergoing Major Abdominal Surgery. Anesth Analg <strong>2011</strong>;112:130-8.28. Gopal S, Jayakumar D, Nelson PN. Meta-analysis on the effect of dopexamine on in-hospital mortality.<strong>Anaesthesia</strong> 2009;64: 589-94.29. Br<strong>and</strong>strup B. Fluid therapy for the surgical patient. Best Practice & Research Clinical Anaesthesiology 2006;Vol. 20(2): 265-283.30. Abbas SM, Hill Ag. Systematic review of the literature for the use of oesophageal Doppler monitor for fluidreplacement in major abdominal surgery. <strong>Anaesthesia</strong>, 2008, 63, pages 44-51.31. Giglio MT, Marucci M, Testini M, Brienza N. Goal-directed haemodynamic therapy <strong>and</strong> gastrointestinalcomplications in major surgery: a meta-analysis of r<strong>and</strong>omized controlled trials. British Journal of <strong>Anaesthesia</strong>2009; 103 (5): 637-46.32. Rahbari NN, Zimmermann JB, Schmidt T, Koch M, Weig<strong>and</strong> MA, Weitz J. Meta-analysis of st<strong>and</strong>ard, restrictive<strong>and</strong> supplemental fluid administration in colorectal surgery. British Journal of Surgery 2009; 96: 331-341.33. Roche AM, Miller TE, Gan TJ. Goal-directed fluid management with trans-oesophageal Doppler. Best Practice& Research Clinical Anaesthesiology. 2009; 23: 327-334.34. Hamilton MA, Cecconi M, Rhodes A. A systematic review <strong>and</strong> meta-analysis on the use of preemptivehemodynamic interventionto improve postoperative outcomes in moderate- <strong>and</strong> high-risk surgical patients.Anesth Analg <strong>2011</strong>; 112:1392-402.35. Miller TE, Roche AM, Gan TJ. Poor Adoption of Hemodynamic Optimization During Major Surgery: Are WePracticing Subst<strong>and</strong>ard Care? Anesth Analg <strong>2011</strong>; 112(6): 1274-6.36. www.nice.org.uk/guidance/MTG3.37. Pogue J, Yusuf S. Overcoming the limitations of current meta-analysis of r<strong>and</strong>omised controlled trials. Lancet1998; 351: 47-52.38. LeLorier J, Grégoire G, Benhaddad A, Lapierre J, Derderian F. Discrepancies between meta-analyses <strong>and</strong>subsequent large r<strong>and</strong>omised, controlled trials. N Engl J Med 1997; 337: 536-542.39. Rigg JRA, Jamrozik K, Myles PS, Silbert BS, Peyton PJ, Parsons RW, Collins KS, for the MASTER <strong>Anaesthesia</strong>Trial Study Group. Epidural <strong>Anaesthesia</strong> <strong>and</strong> Analgesia <strong>and</strong> Outcome of Major Surgery: a R<strong>and</strong>omised Trial.Lancet, 2002; 359: 1276-82.40. Slagt C, Breukers RM, Groeneveld ABJ. Choosing patient-tailored hemodynamic monitoring Critical Care 2010,14:208-13.