Australasian Anaesthesia 2011 - Australian and New Zealand ...
Australasian Anaesthesia 2011 - Australian and New Zealand ...
Australasian Anaesthesia 2011 - Australian and New Zealand ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
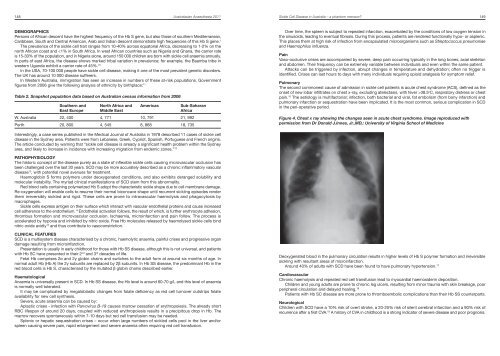
148 <strong>Australasian</strong> <strong>Anaesthesia</strong> <strong>2011</strong>Sickle Cell Disease in Australia – a phantom menace? 149DEMOGRAPHICSPersons of African descent have the highest frequency of the Hb S gene, but also those of southern Mediterranean,Caribbean, South <strong>and</strong> Central American, Arab <strong>and</strong> Indian descent demonstrate high frequencies of this Hb S gene. 1The prevalence of the sickle cell trait ranges from 10-40% across equatorial Africa, decreasing to 1-2% on thenorth African coast <strong>and</strong> 38.5 o C, respiratory distress or chestpain. 16 The aetiology is multifactorial; infection, both bacterial <strong>and</strong> viral, fat embolism (from bony infarction) <strong>and</strong>pulmonary infarction or sequestration have been implicated. It is the most common, serious complication in SCDin the peri-operative period.Figure 4. Chest x ray showing the changes seen in acute chest syndrome. Image reproduced withpermission from Dr Donald J.Innes, Jr.,MD,: University of Virginia School of MedicineInterestingly, a case series published in the Medical Journal of Australia in 1978 described 11 cases of sickle celldisease in the Sydney area. Patients were from Lebanese, Greek, Cypriot, Spanish, Portuguese <strong>and</strong> French origins.The article concluded by warning that “sickle cell disease is already a significant health problem within the Sydneyarea, <strong>and</strong> likely to increase in incidence with increasing migration from endemic zones.” 12PATHOPHYSIOLOGYThe historic concept of the disease purely as a state of inflexible sickle cells causing microvascular occlusion hasbeen challenged over the last 30 years. SCD may be more accurately described as a chronic inflammatory vasculardisease 13 , with potential novel avenues for treatment.Haemoglobin S forms polymers under deoxygenated conditions, <strong>and</strong> also exhibits deranged solubility <strong>and</strong>molecular instability. The myriad clinical manifestations of SCD stem from this abnormality.Red blood cells containing polymerized Hb S adopt the characteristic sickle shape due to cell membrane damage.Re-oxygenation will enable cells to resume their normal biconcave shape until recurrent sickling episodes renderthem irreversibly sickled <strong>and</strong> rigid. These cells are prone to intravascular haemolysis <strong>and</strong> phagocytosis bymacrophages.Sickle cells express antigen on their surface which interact with vascular endothelial proteins <strong>and</strong> cause increasedcell adherence to the endothelium. 14 Endothelial activation follows, the result of which, is further erythrocyte adhesion,thrombus formation <strong>and</strong> microvascular occlusion. Ischaemia, microinfarction <strong>and</strong> pain follow. The process isaccelerated by hypoxia <strong>and</strong> inhibited by nitric oxide. Free Hb molecules released by haemolysed sickle cells bindnitric oxide avidly 15 <strong>and</strong> thus contribute to vasoconstriction.CLINICAL FEATURESSCD is a multisystem disease characterised by a chronic, haemolytic anaemia, painful crises <strong>and</strong> progressive org<strong>and</strong>amage resulting from microinfarction.Presentation is usually in early childhood for those with Hb SS disease, although this is not universal, <strong>and</strong> patientswith Hb SC have presented in their 2 nd <strong>and</strong> 3 rd decades of life.Fetal Hb comprises 2α <strong>and</strong> 2γ globin chains <strong>and</strong> switches to the adult form at around six months of age. Innormal adult Hb (Hb A) the 2γ subunits are replaced by 2β subunits. In Hb SS disease, the predominant Hb in thered blood cells is Hb S, characterised by the mutated β globin chains described earlier.HaematologicalAnaemia is universally present in SCD. In Hb SS disease, the Hb level is around 60-70 g/L <strong>and</strong> this level of anaemiais normally well tolerated.It may be complicated by megaloblastic changes from folate deficiency as red cell turnover outstrips folateavailability for new cell synthesis.Severe, acute anaemia can be caused by:Aplastic crises - infection with Parvovirus B-19 causes marrow cessation of erythropoiesis. The already shortRBC lifespan of around 20 days, coupled with reduced erythropoiesis results in a precipitous drop in Hb. Themarrow recovers spontaneously within 7-10 days but red cell transfusion may be needed.Splenic or hepatic sequestration crises – occur when large numbers of sickled cells pool in the liver <strong>and</strong>/orspleen causing severe pain, rapid enlargement <strong>and</strong> severe anaemia often requiring red cell transfusion.Deoxygenated blood in the pulmonary circulation results in higher levels of Hb S polymer formation <strong>and</strong> irreversiblesickling with resultant areas of microinfarction.Around 40% of adults with SCD have been found to have pulmonary hypertension. 17CardiovascularChronic haemolysis <strong>and</strong> repeated red cell transfusion lead to myocardial haemosiderin deposition.Children <strong>and</strong> young adults are prone to chronic leg ulcers, resulting from minor trauma with skin breakage, poorperipheral circulation <strong>and</strong> delayed healing. 18Patients with Hb SC disease are more prone to thromboembolic complications than their Hb SS counterparts.NeurologicalChildren with SCD have a 10% risk of overt stroke, a 20-25% risk of silent cerebral infarction <strong>and</strong> a 90% risk ofrecurrence after a first CVA. 19 A history of CVA in childhood is a strong indicator of severe disease <strong>and</strong> poor prognosis.