Australasian Anaesthesia 2011 - Australian and New Zealand ...
Australasian Anaesthesia 2011 - Australian and New Zealand ...
Australasian Anaesthesia 2011 - Australian and New Zealand ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
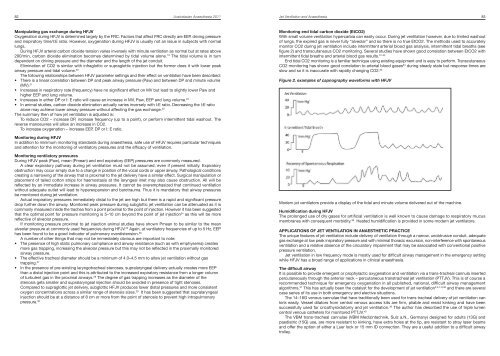
82 <strong>Australasian</strong> <strong>Anaesthesia</strong> <strong>2011</strong>Jet Ventilation <strong>and</strong> <strong>Anaesthesia</strong> 83Manipulating gas exchange during HFJVOxygenation during HFJV is determined largely by the FRC. Factors that affect FRC directly are EEP, driving pressure<strong>and</strong> inspiratory time/I:E ratio. However, oxygenation during HFJV is usually not an issue in subjects with normallungs.During HFJV arterial carbon dioxide tension varies inversely with minute ventilation as normal but at rates above200/min, carbon dioxide elimination becomes determined by tidal volume alone. 19 The tidal volume is in turndependent on driving pressure <strong>and</strong> the diameter <strong>and</strong> the length of the jet conduit.Elimination of CO2 is similar with infraglottic or supraglottic injection but the former does it with lower peakairway pressure <strong>and</strong> tidal volume. 20The following relationships between HFJV parameter settings <strong>and</strong> their effect on ventilation have been described:• There is a linear correlation between DP <strong>and</strong> peak airway pressure (Paw) <strong>and</strong> between DP <strong>and</strong> minute volume(MV). 21• Increases in respiratory rate (frequency) have no significant effect on MV but lead to slightly lower Paw <strong>and</strong>higher EEP <strong>and</strong> lung volume.• Increases in either DP or I: E ratio will cause an increase in MV, Paw, EEP <strong>and</strong> lung volume. 22• In animal studies, carbon dioxide elimination actually varies inversely with I:E ratio. Decreasing the I:E ratioalone may achieve lower airway pressure without affecting the gas exchange. 23The summary then of how jet ventilation is adjusted is:To reduce CO2 – increase DP, increase frequency (up to a point), or perform intermittent tidal washout. Thereverse manoeuvres will allow an increase in CO2.To increase oxygenation – increase EEP, DP or I: E ratio.Monitoring end tidal carbon dioxide (EtCO2)With small volume ventilation hypercarbia can easily occur. During jet ventilation however, due to limited washoutof lungs, the expired gas is never fully “alveolar” <strong>and</strong> so there is no true EtCO2. The methods used to accuratelymonitor CO2 during jet ventilation include intermittent arterial blood gas analysis, intermittent tidal breaths (seefigure 2) <strong>and</strong> transcutaneous CO2 monitoring. Several studies have shown good correlation between EtCO2 withintermittent tidal breaths <strong>and</strong> arterial blood gas results. 31-33End tidal CO2 monitoring is a familiar technique using existing equipment <strong>and</strong> is easy to perform. TranscutaneousCO2 monitoring has shown good correlation to arterial blood gases 34 during steady state but response times areslow <strong>and</strong> so it is inaccurate with rapidly changing CO2. 35Figure 2. examples of capnography waveforms with HFJVMonitoring during HFJVIn addition to minimum monitoring st<strong>and</strong>ards during anaesthesia, safe use of HFJV requires particular techniques<strong>and</strong> attention for the monitoring of ventilatory pressures <strong>and</strong> the efficacy of ventilation.Monitoring ventilatory pressuresDuring HFJV peak (Paw), mean (Pmean) <strong>and</strong> end expiratory (EEP) pressures are commonly measured.A clear expiratory pathway during jet ventilation must not be assumed, even if present initially. Expiratoryobstruction may occur simply due to a change in position of the vocal cords or upper airway. Pathological conditionscreating a narrowing of the airway that is proximal to the jet delivery have a similar effect. Surgical manipulation orplacement of tailed cotton strips for haemostasis at the laryngeal inlet may also cause obstruction. All will bereflected by an immediate increase in airway pressures. It cannot be overemphasized that continued ventilationwithout adequate outlet will lead to hyperexpansion <strong>and</strong> barotrauma. Thus it is m<strong>and</strong>atory that airway pressuresbe monitored during jet ventilation.Actual inspiratory pressures immediately distal to the jet are high but there is a rapid <strong>and</strong> significant pressuredrop further down the airway. Monitored peak pressure during subglottic jet ventilation can be attenuated as it iscommonly measured inside the trachea from a point proximal to the point of injection. However it has been suggestedthat the optimal point for pressure monitoring is 5–10 cm beyond the point of jet injection 24 as this will be morereflective of alveolar pressure.If monitoring pressure proximal to jet injection animal studies have shown Pmean to be similar to the meanalveolar pressure at commonly used frequencies during HFJV. 25 Again, at ventilatory frequencies of up to 5 Hz, EEPhas been found to be a good indicator of pulmonary overdistension. 26A number of other things that may not be immediately obvious are important to note:• The presence of high static pulmonary compliance <strong>and</strong> airway resistance (such as with emphysema) createsmore gas trapping, increasing the alveolar pressure but this may not be reflected in the proximally monitoredairway pressure.• The effective tracheal diameter should be a minimum of 4.0–4.5 mm to allow jet ventilation without gastrapping. 27• In the presence of pre-existing laryngotracheal stenoses, supralaryngeal delivery actually creates more EEPthan a distal injection point <strong>and</strong> this is attributed to the increased expiratory resistance from a longer columnof turbulent gas in the proximal airways. 28 The degree of gas trapping increases as the diameter of thestenosis gets smaller <strong>and</strong> supralaryngeal injection should be avoided in presence of tight stenoses.Compared to supraglottic jet delivery, subglottic HFJV produces lower distal pressures <strong>and</strong> more consistentoxygen concentrations across a similar range of stenosis sizes. 29 It has been suggested that supralaryngealinjection should be at a distance of 8 cm or more from the point of stenosis to prevent high intrapulmonarypressure. 30Modern jet ventilators provide a display of the tidal <strong>and</strong> minute volume delivered out of the machine.Humidification during HFJVThe prolonged use of dry gases for artificial ventilation is well known to cause damage to respiratory mucusmembranes with consequent morbidity. 36 Heated humidification is provided in some modern jet ventilators.APPLICATIONS OF JET VENTILATION IN ANAESTHETIC PRACTICEThe unique features of jet ventilation include delivery of ventilation through a narrow, unobtrusive conduit, adequategas exchange at low peak inspiratory pressure <strong>and</strong> with minimal thoracic excursion, non-interference with spontaneousventilation <strong>and</strong> a relative absence of the circulatory impairment that may be associated with conventional positivepressure ventilation.Jet ventilation in low frequency mode is mostly used for difficult airway management in the emergency settingwhile HFJV has a broad range of applications in clinical anaesthesia.The difficult airwayIt is possible to provide emergent or prophylactic oxygenation <strong>and</strong> ventilation via a trans-tracheal cannula insertedpercutaneously through the anterior neck – percutaneous transtracheal jet ventilation (PTTJV). This is of course arecommended technique for emergency oxygenation in all published, national, difficult airway managementalgorithms. 37 This has actually been the catalyst for the development of jet ventilation 3,5,7-9,38 <strong>and</strong> there are severalcase series of its use in both emergency <strong>and</strong> elective situations.The 14–16G venous cannulae that have traditionally been used for trans tracheal delivery of jet ventilation cankink easily. Vessel dilators from central venous access kits are firm, pliable <strong>and</strong> resist kinking <strong>and</strong> have beensuccessfully used for cricothyroidotomy <strong>and</strong> jet ventilation. 39 The author has described the use of triple lumencentral venous catheters for monitored PTTJV. 40The VBM trans-tracheal cannulae (VBM Medizintechnik, Sulz a.N., Germany) designed for adults (13G) <strong>and</strong>paediatric (15G) use, are more resistant to kinking, have extra holes at the tip, are resistant to stray laser beams<strong>and</strong> offer the option of either a Luer lock or 15 mm ID connection. They are a useful addition to a difficult airwaytrolley.